The COVID Vaccines, Booster Shots and How Medical Advances Are Made
( AP Photo )
[music]
Brian Lehrer: It's The Brian Lehrer Show on WNYC. Good morning again, everyone. With all the vaccine booster news right now, I'm very glad to have Dr. Paul Offit with us. He's a member of the FDA's Vaccines and Related Biological Products Advisory Committee. You know about the FDA advisors voting to recommend for now that third doses be allowed only for people over 65 or with certain underlying conditions, or for healthcare workers or others whose jobs put them at risk for COVID exposure. You know this is only for those who got the Pfizer vaccine for now. Maybe you heard today's news that Johnson and Johnson released a study showing an additional shot of its vaccine substantially boosts its effectiveness.
Dr. Offit recently said he felt the timing of all this was being rushed to meet an artificial timeline set by the President. Of course, a number of other countries are already giving boosters, and then there's the approval being considered for first dose vaccines for children as young as five. Dr. Offit also has a new book that he started writing before the pandemic but that puts a lot of this into a fascinating historical context. It's called You Bet Your Life: From Blood Transfusions to Mass Vaccination, the Long and Risky History of Medical Innovation. We'll talk about the news, we'll talk about the book, we'll talk about where they fit together in his day job.
Dr. Paul Offit is director of the Vaccine Education Center at the Children's Hospital of Philadelphia. Dr. Offit, so good to have you today. Thanks for coming on WNYC.
Dr. Paul Offit: Thank you, Brian. It's my pleasure.
Brian Lehrer: First, to be clear, are you on the same FDA Vaccine Advisory Committee that made the formal recommendation on Friday?
Dr. Paul Offit: Yes, I am.
Brian Lehrer: I saw you said on CNN that you think this is being rushed to fit President Biden's artificial timeline after he said this summer that boosters would be available starting September 20th, which was yesterday. Do you think the science isn't there for any of this yet?
Dr. Paul Offit: Well, no, I wouldn't say that. I think by setting a September 20th deadline and saying this is going to happen on September the 20th, you're going to get a third dose, it will be available for the general population, it'll be eight months after the first dose, I don't think he necessarily got ahead of the science as much as he got ahead of the scientific process.
I mean, there is a process here. In theory, you have a problem, the problem being waning immunity, you have a solution, which is a booster dose, you have data that show that that's a solution. Then you submit those data to the Food and Drug Administration which is a regulatory body, and then allows you to distribute then the vaccine under certain guidelines, and then it goes to the CDC which is a recommending body and we're still waiting for that recommendation, hopefully, have it by the end of the week, in terms of who exactly would most benefit from the booster dose. They sidelined the FDA, sidelined the CDC, which I think is never a good idea.
Brian Lehrer: A number of countries in Europe plus Israel in the Middle East are well into vaccine booster distribution. Are you saying that's too political over there and not science-based enough?
Dr. Paul Offit: Well, what's the goal of the vaccine? The goal of vaccines as stated by Dr. Rochelle Olinsky and others is to prevent serious illness. The immunological mechanism of preventing serious illness is something called immunological memory cells, memory B cells, memory T cells. A number of investigators, John Wherry at Penn, Shane Crotty at the La Jolla, and others have found that not surprisingly, memory cells are long-lived.
All the data generated in the United States suggests that's true because if you look, at least in this country, at the capacity of two doses of mRNA containing vaccine to prevent serious illness, you find that it remains high, it remains high against Delta, it remains high for all age groups. The data that we're seeing here do not really reflect what's being seen in Israel. Do you really want to use an Israeli experience to determine how you're going to practice medicine in the United States?
At least regarding prevention of serious illness, the vaccine seems to be holding up. What has eroded is what you would expect to erode at some level which is neutralizing antibodies start to decline after two doses of mRNA vaccine. With that, you get a greater risk of asymptomatic infection, mildly symptomatic infection, even low moderately symptomatic infection associated with increased contagiousness. There you can argue that to give a booster dose will, in theory, decreased to some extent the contagiousness of this virus and therefore the spread of this virus.
That's really the question, to what extent a booster dose for the over 65 group, a booster dose for people who are at high risk is going to change the arc of this pandemic as compared to what everybody agrees is going to change the arc of this pandemic, which is vaccinating people who are unvaccinated. At our hospital, we see people come into the ICU, into the intensive care unit. It's not because they didn't get their third dose, it's because they've never gotten any dose and so that's really an issue.
Brian Lehrer: Do you see a zero-sum game issue of boosters for the United States preventing initial shots around the world, therefore, slowing the defeat of the pandemic overall?
Dr. Paul Offit: Well, that would be sad. I mean, I hope that's not the way it works out. Certainly, we have pledged or given about 100 million doses so far, but you could argue that all the doses that were being given now in this we are about to give or have given as a third dose, would be better served in another country. Because certainly, it's a worldwide pandemic, we know that these variants are being created in other countries. Delta at least was first detected in India, the Alpha variant first detected in the United Kingdom. What happens in this world does affect us, so it's not an altruistic act to give vaccines to the developing world.
The WHO has been somewhat critical about giving third doses in this situation. Dr. Fauci and the public health advisors to the administration believe that by giving a third dose, that we can change the arc of this pandemic. We'll see. I hope they're right. I hope that's true, but I think we all would agree that if we really want to change the arc of this pandemic, it's about taking that roughly 60 to 65 million people in this country who are simply refusing to get a vaccine and vaccinate them.
Brian Lehrer: Yes. You and others have said the science supports boosters for people 60 and over. The official recommendation that came down from your committee last Friday starts with age 65. What happened to those five additional years?
Dr. Paul Offit: I think where that came from was that in Israel, that's their observation. That there started to be a waning of protection against serious disease in those greater than 60. That's not what we're seeing in the US, in the US it's still even in people over 65, there appears to be protection. I'm not sure there's a critical difference there. In my mind, recommending a third dose for people over 65, frankly, is the same thing as recommending a third dose for those who are immune-compromised, which we've already done. Because as you get older and you're over 65, your immune system is more senescent, and so your capacity to make a robust immune response isn't as good, so that's really how I put the greater than 65-year-old, someone in the immune-compromised category.
Brian Lehrer: New this morning, Johnson and Johnson's just released data showing very strong protection with a second shot. Of course, that's been a one-shot vaccination. How long should J&J recipients have to wait, especially given the slightly lower protection that the J&J seemed to give, to begin with for approval for them?
Dr. Paul Offit: Right. It's interesting, when we, the FDA Vaccine Advisory Committee, met at the end of February to discuss the J&J vaccine, you could see that they had done some two-dose vaccine work. They'd done it preclinically in non-human primates, and you clearly saw there was a two and a half to three-fold increase in neutralizing antibody titers. That was also true in their so-called phase one trials in people. It was not surprising then that a second dose would associate it with that increase in neutralizing antibodies now apparently has been associated with increased effectiveness.
J&J sold themselves as a one-dose vaccine, and that was the advantage. It looks like there's an additional advantage to the second dose, but again, those data have to be submitted to the FDA, reviewed by the FDA, then go to the CDC. I think we're still talking about at least a few weeks till we get clear evidence or a clear recommendation from the CDC on the second dose for J&J's vaccine.
Brian Lehrer: By the way, did you see Cedric the Entertainer on the Emmys Sunday night say that Pfizer is like the Neiman Marcus of vaccines, Moderna is the Macy's, and Johnson and Johnson, that's TJ Maxx? I know it's a comedy, but was he being fair to J&J?
Dr. Paul Offit: I don't think so. I think if you look at the capacity of one dose of J&J's vaccine to induce memory cells, it's excellent. The capacity of J&J to protect against serious disease is also excellent, and it was an advantage as a single dose. I think now we're starting to focus on something that's going to be a lot harder to get in control which is this notion of trying to prevent shedding, meaning asymptomatic shedding or mildly symptomatic shedding. That is a high bar for a vaccine.
I think if I could go back and do this all over again, the one thing I would love to see not happen is to use the term breakthrough illness to describe an asymptomatic infection or mildly symptomatic infection. That's just not fair. I mean, that holds this vaccine to way too high of a standard. Most of the vaccines we have out there, whooping cough vaccine, influenza vaccine, rotavirus vaccine, the job of those vaccines is to prevent severe illness, to prevent hospitalization, ICU admission, death and deaths, those vaccines do that, but they certainly aren't very good about preventing asymptomatic infection or mildly symptomatic infection, and it would be unfair to call those infections breakthrough infections with those illnesses.
Brian Lehrer: Dr. Paul Offit with us from the Children's Hospital of Philadelphia and the FDA Vaccine Advisory Committee that approved the booster dose for the populations we've been discussing on Friday. Your book is called You Bet Your Life: From Blood Transfusions to Mass Vaccination, the Long and Risky History of Medical Innovation. Why do you focus on the intersection between innovation and risk?
Dr. Paul Offit: Because it's always there. We learn as we go, there's a learning curve and there is invariably a human price for knowledge. That's true here with this vaccine. I think, with the mRNA vaccines, there was never any indication in preclinical studies in experimental animals, or in the phase one or two or three studies even involving tens of thousands of people that myocarditis would have ever been a problem, but it is a problem primarily in the 16 to 17-year-old male who gets this vaccine or that the J&J or AstraZeneca vaccines would be associated with a severe clotting problem, including something called cerebral venous sinus thrombosis, which is basically a blood clot in your brain.
I think you learn as you go, and I do think we're intolerant of that, that we'd like to believe we know everything at a particular point of time, but we don't. The question is never when do you know everything, it's when do you know enough? This came up for me actually, this being on the FDA Vaccine Advisory Committee with regard to the 12 to 15-year-old vaccine recommendation. That was a 2,300 child study. Half were given vaccine, half were given placebo. There were 18 cases of COVID in those children 12 to 15 years of age, all in the placebo group. That vaccine then was permitted under emergency use authorization to be given to the 12 to 15-year-old.
I got a lot of angry emails from people saying 2,300 children, that's all you want to study? Don't you want to study more than that? Why not study 23,000, making it a little closer to what we did for the adults? You can do a 23,000 child study and then presumed there wouldn't have been 18 cases of COVID in the placebo group, there may have been 180 cases. When do you pull the trigger? When do you cross the line and that's what I do in this book is go through the nine major medical advances that have caused us to live 30 years longer now than we did 100 years ago and it stopped at various points in time and say, all right, would you get it now? Would you get it now?
Then the story continues and you could see basically, it's one tragedy after another as we move forward. We learn as we go on, it's that knowledge that is invariably hard-earned.
Brian Lehrer: One of your chapters is about the initial rollout of the polio vaccine, which you also wrote a whole separate book about I know a few years ago, and that rollout was controversial. Now we accept the polio vaccine unquestioningly, so what happened then, and does it relate to now?
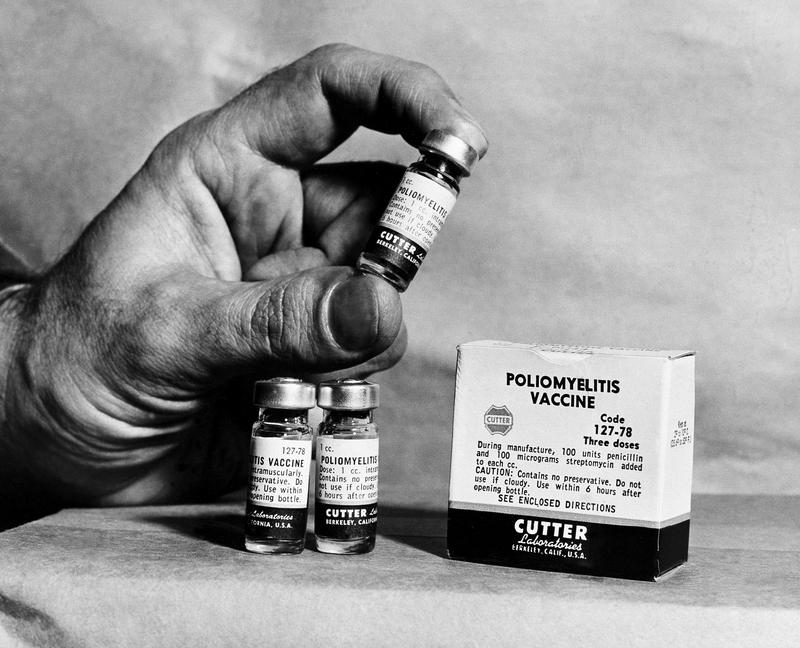
Dr. Paul Offit: Well, there were two things that were interesting there. One is that so Jonas Salk made his polio vaccine by taking poliovirus, growing it up in cell culture, purifying the virus, and then inactivating the virus with a chemical, that's the way he made it. Five companies stepped forward to make that vaccine, to mass-produce it and distribute it. One of them made it badly. Cutter Laboratories of Berkeley, California failed to fully inactivate the virus. As a consequence, 120,000 children were inoculated with live, fully virulent poliovirus. 40,000 developed abortive or short-lived polio, meaning temporary paralysis, 164 were permanently paralyzed, and 10 were killed.
I think it's probably one of the worst biological disasters in this country's history, but it didn't flow and so we learned from it. We learned about how to mass-produce that vaccine and that was a remarkable tragedy. There was another tragedy there that was hidden that I think people didn't pay attention to and it's this. The trial that was done, the study that was done to test Jonas Salk's vaccine broke his heart. It's not what he wanted to do. He had made his vaccine, he'd tested it in 700 children in the Pittsburgh area. He said, "Eureka, I've got it. The vaccine is safe and it works."
The March of Dimes and the federal government wanted to do a big study to prove that it worked. They gave the vaccine to 420,000 children. These are first and second graders in the 1950s. I was a first and second grader in the 1950s, and they gave 200,000 placebo doses to children in the first and second grade. He could not conscience giving saltwater to children as we entered the summer during a polio epidemic and so what ended up happening was the vaccine was declared safe, potent, and effective but how do we know it was effective?
We knew was effective because 16 children died in that study, all in the placebo group of polio. We knew it was effective because 36 children were paralyzed permanently in that study, 34 in the placebo group but for the flip of a coin, those children would be my age now and could have lived a long healthy, and productive life. Again, you learn as you go, and again, always what price knowledge.
Brian Lehrer: That's why even with some risk, you approve at a certain point if you've got that other side of the data like those, that concentration of deaths in the placebo group. A non-vaccine example from your book was the introduction of blood transfusions. Can you tell us a little bit of that story, the dramatic innovation, and the risks in that case?
Dr. Paul Offit: Sure. The way I tell that story is say, okay, would you get a blood transfusion now? You start a couple of hundred years ago when we basically were transfusing blood from farm animals into people. Would you get a blood transfusion then? Then you move to the early 1900s and we identify blood types, the A, B, O blood categories. Would you get a vaccine would you get a blood transfusion now? We still hadn't identified yet the so-called Rh factor, so your O positive, O negative, that positive or negative is the Rh factor. Then you know about the Rh factor, would you get a blood transfusion now?
Then what happens is human immunodeficiency virus, the AIDS virus enters the blood supply and kills tens of thousands of people who got contaminated blood transfusions. Okay, would you get a blood transfusion now, knowing that there are many viruses for which we don't test the whole blood? Knowing that there are viruses we don't yet know about, would you get it now? Knowing that there are risks there, would you be one of the first to volunteer for artificial blood, which is currently being tested in the laboratory? When do you feel you know enough to make the right decision?
Another example would be heart transplants. There's 4000 people currently waiting for a heart transplant in this country. 1300 will die while waiting. Do want to be one of the first people to get a pig heart as a transplant? That's what this book is about. It's about when do you know enough to say, "Okay, I want to enter this medical innovation now."
Brian Lehrer: Janet in Manhattan, you're on WNYC with Dr. Paul Offit. Hi, Janet.
Janet: Oh, hi. Thank you very much. First of all, I'm confused, when we say that-- Two levels to this question, one is when we say the FDA approved the vaccine or approved the drug, how many people are we talking about here? Who gets to vote on it? Is it the Supreme Court where they say, well, five of us are in favor, and four are against so it's approved? The reason I'm asking is I heard a very disturbing story on NPR, that two very high profile members of the FDA, I guess voting members, so strongly disagreed with the decision made by the majority on the FDA that they publicly resigned.
They were being interviewed or the reporter on this was being interviewed on NPR and somebody said, "Oh, people come and go from the FDA all the time," and the other reporter said, "Wait a minute, these were not just people, these were the highest-profile specialists in vaccines and they felt strongly enough about the decision that the FDA made, they disagreed with it strongly enough that they resigned publicly."
Brian Lehrer: Janet, thank you. I'm sure you know those scientists, Dr. Offit. How would you tell that story?
Dr. Paul Offit: Here's the story. There are 18 voting members on the FDA Vaccine Advisory Committee. Those voting members are not affiliated with the FDA, they're not affiliated with any pharmaceutical companies, they are independent, and so we voted then ultimately to approve booster dosing in a limited manner. The two people that resigned, Marion Gruber and Phil Krause worked for the FDA, they were senior officials at the FDA, they resigned before we ever had that vote.
They resigned because they didn't like the process as you alluded to earlier, Brian, where basically a date was set, I think they felt that the FDA's arm was being twisted to approve the vaccine as a third dose for everybody who was going to be over 16 years of age and they didn't like that. Basically, this resignation was a protest for that, but it really had nothing to do with the booster vote per se, this all happened before the booster.
I think my guess is that they would approve of the way the booster vote played out because we really rejected the Biden's administration desire and I think Pfizer's desire to give this vaccine to the general population, to everybody over 16 as a booster dose. I think they probably would have approved of that outcome.
Brian Lehrer: A follow up on that, and I know you have to go in a minute, the vaccine approval process for 5 to 11-year-olds, what would you need to see to decide that safe for the developing bodies of that age group, and do you assess it differently from vaccines for adults? This plays into the risk versus benefit formula that's the premise of your book too.
Dr. Paul Offit: Exactly, so you want to see, first of all, how they came to the conclusion that they were giving not 30 micrograms of messenger RNA but 10 micrograms, so a third of the dose as two separate doses, again, three weeks apart. We look at the so-called phase one dose-ranging data to see how they came to that conclusion. Two, to look most importantly at safety, safety, safety. Look at every child to see whether or not there were any safety issues and whether they had the same problems with really the second dose associated with fever, headache, fatigue, joint like muscle ache.
Three, look at the consistency of the responses to make sure that it wasn't like 80% or 85% that we're having good antibody responses, but it was closer to 100%. You really need to see the data. Right now, again, we're in the era of science by press release so we're just looking at top-line data provided by the company. We really need to look at the details and with that, then we'll do what we always do, which is that if we say yes, we would allow this vaccine to be distributed to 5 to 11-year-olds, what we're really really saying is would we give it to our own children or nieces or nephews or grandchildren? That's really the bar that we hold every vaccine to.
Brian Lehrer: Well, that's right. What would you say to parents who may have rushed to get a vaccine for themselves but say my six-year-old, I don't know.
Dr. Paul Offit: Well, that's what they always say. We see our children as more vulnerable, but I think, and this is the theme of the book too, is that there are no risk-free choices, there's just choices that take different risks. I think your job is to in the most clear-eyed dispassionate way possible choose the lesser risk.
Brian Lehrer: Dr. Paul Offit's new book is You Bet Your Life: From Blood Transfusions to Mass Vaccination, the Long and Risky History of Medical Innovation. If you want to see him in a virtual town hall, it will be next Wednesday, September 29th, sponsored by the Seattle Town Hall. There's a $5 fee to attend virtually except it's free if you're 22 years old or under. Again, Seattle Town Hall next Wednesday, September 29th, 9:00 PM Eastern Time virtual event with Dr. Paul Offit. Thank you so much for joining us today. I really enjoyed it.
Dr. Paul Offit: Thank you, Brian.
Brian Lehrer: Brian Lehrer on WNYC, more to come.
Copyright © 2021 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.

