Ivermectin Facts and Myths
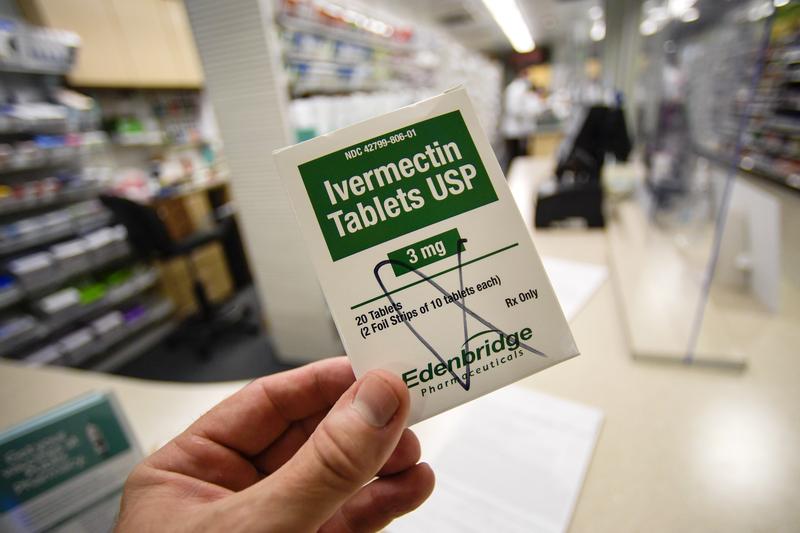
( Mike Stewart / AP Photo )
[music]
Brigid Bergin: It's the Brian Lehrer Show on WNYC. Welcome back, everybody. I'm Brigid Bergin from the WNYC and Gothamist newsroom. All this week, Brian has been tackling various COVID-19 and vaccine myths from the false fear that vaccines are harmful to pregnant women to the idea that the vaccine itself can give you COVID-19. Well, today, we wanted to tackle the topic of ivermectin and other therapies being promoted as alternatives to vaccination.
More than a year and a half into the pandemic, various drugs have had their moments in the anti-vax circles, and ivermectin is not particularly different than, say, hydroxychloroquine, but its popularity comes at a particularly high-stakes time when parts of the country are experiencing yet another COVID wave, and the president has made it a national priority to get vaccination numbers up, so what does the science actually say about this anti-parasitic drug and how did it get so popular?
With me now to talk about both of these questions are Dr. Amesh Adalja, infectious disease doctor and senior scholar at the Johns Hopkins University Center for Health Security, and Tara Haelle, science journalist who covers vaccine hesitancy and the anti-vaccine movement and the author of the book for young readers, Vaccination Investigation: The History and Science of Vaccines. Dr. Adalja and Tara, welcome to WNYC.
Tara Haelle: Hi, thank you.
Dr. Adalja: Thanks for having me.
Brigid Bergin: Ivermectin has been flippantly described as just a drug for deworming horses, which it is, but that's not a fair or complete description, there are formulations of it that are meant for humans, and it's used on humans to treat parasites. Aside from this new notorious life as an unproven COVID therapy, what is ivermectin used for in humans, doctor?
Dr. Adalja: Ivermectin is a very important anti-parasitic drug. We use it for certain types of worm infections, we use it for scabies, and it's something that's on the WHO Essential Medications List. It's something that the discovery of which led to a Nobel Prize, so it is a real drug, it's just that it does not have strong efficacy against COVID-19. It's taken on kind of a life of its own, and that's not where its use is. When people dismiss ivermectin, I think it's important to recognize that this is an important infectious disease drug that we use in humans and that just because it's used in veterinary medicine doesn't mean it doesn't have a role in human medicine, it's just not a role that includes COVID-19.
Brigid Bergin: How did it come to be considered as a treatment for COVID and what about its chemistry even made doctors examine that as a possibility?
Dr. Adalja: It started because there was in vitro activity, meaning in a laboratory setting, in a petri dish, that this compound, ivermectin, had antiviral activity. That's an important point to know, because that gives you a lead, can this be something you could repurpose to use for COVID-19, similar to what happened with hydroxychloroquine, and because it was a drug that was already available, that people had experience using, there was a lot of excitement that this might be an easy solution, a low-hanging fruit, so to speak, to use against COVID-19.
What we've seen in many of the trials is that ivermectin really can't hold up when it comes to treating actual patients in terms of the dosing, in terms of does this actually get people better faster? Does this prevent complications? None of the studies that have been definitive, and the ones that have purported to show a positive benefit have been really poor in terms of their quality, in terms of their rigor, and you can't really draw a conclusion from them.
In ones that are done very well, like the one that was published in JAMA in outpatients, didn't really show a benefit, and I think we're still waiting for a definitive trial to show that this actually works, but for now, this is not something I would recommend to my patients. It's something that the guidelines from the NIH, from the Infectious Disease Society of America do not endorse.
Brigid Bergin: Yet there are some countries that have considered it as a legitimate COVID treatment, in Peru, Bolivia, Brazil, Zimbabwe, they added it to their national treatment guidelines. What were those countries responding to in terms of what data and have we gotten any data back from these countries that are officially using it as a treatment?
Dr. Adalja: Countries are interested in having a cheap and easy solution to COVID-19, especially when we don't have any kind of drug that works in an outpatient setting. We don't have a Tamiflu equivalent for COVID-19, so if this is something that would work, because it was cheap, because it was widely available, because it was already approved for other uses, it was an easy solution for many of these countries to use. There was enthusiasm around it, and there was mixed data, not very high quality, that people were using, plus a lot of anecdotal evidence.
We know throughout this pandemic, anecdotal evidence has often been substituted for rigorous clinical trials, really to the detriment of everyone, but that's something that people kind of have a bias towards. When they hear people getting better, they want to use it even if it's not something that has definitively been proven to be effective. I think that drove a lot of it.
We have not seen strong data there that's unequivocal, that has a really strong control arm, that really delves into whether or not this is working in a rigorous randomized controlled trial format, and I think that's been the conundrum, is that many people in South and Central America have used ivermectin, we don't really have much data, and we couldn't do the trials in those areas because so many people wanted it, that they weren't going to enter into a clinical trial where they might get randomized to the placebo group.
In effect, some of that enthusiasm actually made it harder to actually get to the bottom of this because no one wanted to be randomized to a placebo if ivermectin was widely available and being prescribed by doctors all over their country. This is just another example of how many countries got this wrong on the pandemic in a very similar fashion to hydroxychloroquine.
We are waiting for more data, but none of it really looks promising thus far and the one meta-analysis or this big conglomeration of studies that purported to show the benefit was fraudulent, it had to be removed. I think that there's just a lot of conspiracy theories around ivermectin, but the bottom line is, we don't have data to support its use.
Brigid Bergin: Listeners, do you have a question about the science of ivermectin or alternative unproven COVID-19 therapies for my guest, infectious disease Dr. Amesh Adalja, or maybe you know someone who's bought these drugs instead of taking the vaccine. Where did they buy ivermectin and how did they hear about it? I'm also talking to Tara Haelle, a science journalist who covers vaccine hesitancy in the anti-vaccine movement. The number is 646-435-7280.
Tara, you study the history of vaccines and the anti-vaccine movement, for those of us paying attention, we've seen hydroxychloroquine and now we see ivermectin, but what are some of the earlier pre-pandemic examples of this same push for alternative treatments to diseases where vaccines exist?
Tara Haelle: Well, you could see examples of-- I'm trying to think of something. The specific example you just said, a lot of people would create fake flu vaccines, like the things considered natural, they would have, this is not a treatment for a vaccine preventable disease, but you saw something called chelation, it was the removal of heavy metals from children who had been diagnosed with autism.
There's been various types of snake oil over the years forever. Vitamins are often a very popular one, you'll see people say, "Okay, you can treat measles with vitamin C," for example, and it's true that vitamin C is important when you're treating [unintelligible 00:08:11], but it's not a cure for measles, so vitamins are often very popular. Anything that's in sort of the natural, herbal sphere, has probably been used at some point or another to try and treat a disease even if there is not good evidence that it actually can do so.
Brigid Bergin: I think traditionally when people think about, people who are skeptical of vaccines, they would talk about wanting to keep everything that they put into their bodies pure, but if your concern is safety and you don't trust Big Pharma, how does ivermectin fit into that? It's not like it's some benign wellness tincture, it's also a pharmaceutical product, so how do you thread that needle?
Tara Haelle: Well, you're trying to make something logical out of a belief system, and there's not a logical answer to that, it's plain old, that cognitive dissonance that happens. If they have seen evidence that they think is being repressed in some way or suppressed, which is what they're believing, they think that it's being hidden, that it's a very inexpensive drug, it's available in other places, they're seeing other countries that are pulling it, that are using it or claiming to use it, they're going to see that as part of some big conspiracy that is trying to prevent people in the United States from using it because they want to push the big vaccines from the big companies.
It's not necessarily logical, but it's ideological, and so it's trying to make sense of that in a logical way, you can't do it. There's not the evidence for it, but we've seen lots of examples in the anti-vaccine movement where the belief system doesn't make sense, but that's not part of what it's about, it's an ideological idea.
Brigid Bergin: Let's go to the phones. Krishna in Brooklyn. Krishna, welcome to WNYC. Do you have a question or a comment on this debate over ivermectin?
Krishna: Hi. Yes, I do. Thanks so much for taking my call. I'm actually an emergency medicine doctor. I live in Brooklyn. I have a couple of questions actually, but real quick, one of the questions is, I don't know-- who are these doctors that are actually prescribing such a thing like ivermectin? No matter how much the patient asks for, I personally would never do it no matter how much a patient begged, and I would do my best to explain that it's not appropriate.
Are these doctors subject to any possible sanction in any way for doing something that's not proven in any way? Also, my other question is, a doctor like Pierre Kory who has been promoting this unproven therapy, can you speculate at all as to what his motivations might be for doing that?
Brigid Bergin: Thank you so much, Krishna. Tara, Dr. Adalja, what do you make of Krishna's question about who's prescribing and what the potential implications are?
Dr. Adalja: I can tell you it's not Infectious Disease doctors that are prescribing it by and large. I've heard about urgent care doctors and primary care physicians that are prescribing it. It seems to be kind of a cottage industry where there are certain doctors who have bought into the ivermectin data, and they're the ones that will do it. Sometimes those doctors become popular through word of mouth. I don't know that there's any way to really report them or do anything like that.
I think that there are, you can complain to your State Medical Board if someone is doing non-evidence-based medicine, but doctors have a lot of latitude when it comes to prescribing drugs that are already approved off-label, especially if they're prescribing it in a way that's not causing toxicity. Where we're seeing toxicity [unintelligible 00:11:59] poison centers, happens to be when people get ahold of the veterinary form of it, which may have a different dosage of it.
Lastly, the caller asked about Dr. Pierre Kory who was a very well respected critical care physician. A lot of us don't really understand where this has come from and why he has become the face of it and testified in Congress and become really the fountainhead of what's going on here. I think one of the puzzles is why he has been advocating this even when there's been an absence of data, and he's an academic critical care doctor, and he knows how to evaluate data, and I think it's just another mystery of ivermectin.
Brigid Bergin: Tara, anything you want to add?
Tara Haelle: Not much. We do see this kind of pattern with other doctors. We've seen it-- In every community, there's the doctor who you can go to, who will do the alternative vaccine schedule or the doctor who will see you and won't do vaccines at all and will give you the natural stuff. There's always been doctors that do this. I've written about several of them.
Unfortunately, like the doctor just said, there's not great ways to censure them. Some of them have done some pretty extreme things and are very well known for taking money, cash-only kind of situations, where they can be seen to give this. Some of it might be financially motivated with some of the doctors, but some of the doctors are also true believers, and it's hard to know why, but it's very frustrating. Sometimes you wonder, like the doctor said, this doctor should know better and why? Why, why, why? We don't know.
Tara Haelle: Doctor, there are other treatments that people have talked about as alternatives. I want to talk a little bit more about what and if any of those have scientific merit. Here's a new one, I heard you talking about, gargling with Betadine and antiseptic to treat cuts and scrapes. Where did that idea come from?
Dr. Adalja: I have no idea where that idea came from, because we're talking about an iodine solution that everybody has had put on their cuts and wounds, that if you've had a surgery, that might have been put on your skin before they made the incision, and yes, Betadine is an antiseptic.
Yes, it can kill viruses on contact, but that doesn't translate to ingesting it, and there are some gargling products that have been out there, and in some data, that says yes, that this has an impact on SARS-CoV-2, but all of that-- I think the important part is when you have that kind of data from in vitro studies and small studies and certain selected patient groups, that doesn't translate to that becoming a standardized treatment for it.
I think what we're seeing is people now drinking Betadine, which has iodine in it, which interferes with-- can cause kidney failure, which can cause problems with your thyroid because of all the iodine. I think it's another alternative treatment. That's not a treatment at all, but basically a poison the way it's been used. To me, it's mind-boggling that someone will look at drinking something like that rather than taking a vaccine, which has been put into hundreds of millions of people's arms, and we've seen the risk-benefit ratio with our own eyes, but yet they'll try something like that. They'll put that into their body.
That to me kind of really speaks to the scientific literacy in the United States and how bad it is and how people don't understand what evidence is and what an arbitrary type of assertion is about some treatment that might work because of this rather than a body of evidence that gets evaluated over time and it's peer-reviewed and becomes generally accepted because it works, it's reproducible, all of those principles of the scientific method that you learn in fifth grade science class, I think most of this country has forgotten that.
Brigid Bergin: Another drug I read about this week, fluvoxamine, an antidepressant, is currently being used to treat severe COVID, is that right?
Dr. Adalja: Fluvoxamine, it's an SSRI, a common type of antidepressant drug. There was an initial trial that was published in, I believe, JAMA, that was positive, that showed that there was some benefit in decreasing complications from COVID-19, but it was a small study, and it needs to be followed up. Fluvoxamine does have some data behind it, but again, another thing from the scientific method, just remembering from your fifth grade science class, is reproducibility. You want to see more studies and you want to see them in larger swaths of the population to make sure that this is not a spurious result.
Remember, lots of people in this country already take an antidepressant similar to fluvoxamine and you don't want to be mixing fluvoxamine with Zoloft or Prozac or whatever it might be because you could get a dangerous complication called serotonin syndrome.
This is something that needs to be studied more before it can be operationalized. There is a positive signal there. I'd like to see more studies on fluvoxamine before I would prescribe them, but people shouldn't be doing this on their own, and if they are doing it, make sure you talk to your doctor about other antidepressants that you may be on that could interact and cause a dangerous and deadly reaction called serotonin syndrome if you mix all of these together and overload your body with serotonin.
Brigid Bergin: Go ahead, Tara, were you going to jump in?
Tara Haelle: Yes, I was going to say something about, I don't disagree that scientific literacy is a serious problem in the United States on many levels. At the same time, however, a lot of the trust in these products and the desire to use these products, it's not so much a factor of scientific illiteracy as it is cognitive biases and fear, distrust, a loss of control.
We have to remember that we are rational animals, but our lizard brain developed first. We are often ruled by our emotions before our rational brain even if we want to think that we're more rational, and a lot of people, they're experiencing a lot of fear about the disease. They're also experiencing distrust of the government, and there's been a lot of reasons to distrust the government over the last several years.
It's completely understandable. In the midst of all of that, we have a rapidly changing environment with the pandemic where we're trying to get new information, and the data changes, it's do we wear masks? Do we not wear masks? Can you wear masks with a vaccine? Maybe you shouldn't wear masks with a vaccine. Now you-- We as scientists and science journalists and people who follow that, we understand that we're an looking at the sausage factory really, really close. Our noses are up against the window staring at it.
The general public is not used to seeing the scientific process that close up, so the normal iterative process of science where there's stops and starts and corrections, the whole self-correcting aspect of it is not something they're used to seeing close up. That fosters distrust in an environment that already has a lot of fear and a lot of a sense of loss control. When people are taking these, they're feeling like, "I want to assert control over my own fate" and feeling the certainty of using these products gives them that sense of control.
Brigid Bergin: Let's take one of our callers, Julia in Stamford, Connecticut. Tell us what your experience is with this, and we'll get hopefully a reaction from the doctor who I know has to leave us in just a few moments.
Julia: Hi, everyone. Thanks for taking my call. I got COVID, my family and I got COVID back in December of 2020. I am a COVID long-hauler. I still experience symptoms. It's been a rough go, and it's hopeless, it feels very hopeless and helpless. I found a doctor who works at a very reputable hospital. I'm not going to say his name, but he works at a reputable hospital. He was also a COVID long-hauler, and he prescribed me ivermectin. It might have been like four months into it.
I live at the top of a hill, and I was unable to hardly even walk to my mailbox, but slowly, I tried to walk to the bottom of the hill, and it would take me, like stopping after every step to get to the top. 72 hours after taking the ivermectin, I was able to walk to the top of the hill. This is an anecdotal experience. I don't know if it was the ivermectin, I'm also taking other things, but I feel like the COVID long-haul has kind of been left out of the conversation. I also got vaccinated, but I look forward to more research done on ivermectin and COVID long-haul.
Brigid Bergin: Julia, thank you for sharing your experience. We wish you well as you deal with the long-haul symptoms of that. Doctor, I think it's an important issue that she raised, which is that the long-haulers being left out of the conversation, is something that it seems important to address. Can you speak to whether there are different studies as it relates to treatment for long-haulers and to what extent ivermectin has been part of that?
Dr. Adalja: Long-haul COVID is a major mystery that we're just scratching the surface of. We have a lot of science to do. We actually have to do basic things like coming up with a definition of what long-haul COVID actually is, because there's many definitions and many different studies and we have to really learn to separate which are the symptoms that are debilitating in terms of impair your activities of daily living, your ability to perform your activities of daily living. Then you also have to separate out people who might have had post-ICU syndrome because they had a severe case, because that's a totally different entity, post-ICU syndrome.
Once we-- We're doing that now, I think you're starting to see more people get more specific about what they actually mean by long COVID and that's [unintelligible 00:21:53] research to occur. I think we don't still have a lot of answers. We know that it's more common in females. That the older you are, the more likely you are to have it. The more comorbidities you have, the more likely you are to have it. It's not something that we have enough of a handle on, and there are treatments going on. People are looking at the vascular system and the way your blood pressure is regulated.
There are people looking at medications, ivermectin is something that I wouldn't anticipate it being very beneficial there unless it's having an immune-modulatory effect, meaning changing your immune system. The thing is we can't know anything with just anecdotes. That can be hypothesis-generating. It might be the basis for another study, but I think for ivermectin, even in this situation, you want to do a randomized controlled trial that's rigorously designed to actually show is there a benefit.
Just like the anecdotes of people getting vaccinated that had long COVID getting better, we can't say that's-- anything either. It's based on anecdote. It's great that people feel better, but I don't think you can turn that into a treatment based on that. You need to do rigorous studies to be able to know for sure that this is something that's a real biological effect.
Brigid Bergin: I want to jump in and just for a moment thank Dr. Amesh Adalja for joining us. He's an infectious disease doctor and senior scholar at the Johns Hopkins University Center for Health Security. Dr. Adalja, I know you need to go, and we thank you so much for joining us on the Brian Lehrer Show. We're going to continue the conversation with Tara for a couple more minutes here. Tara, you have written about this shift in the anti-vaccine movement over the past few years where the argument really went from safety to parent choice. I think you traced that evolution to a measles outbreak in 2015. Is that right?
Tara Haelle: That's correct, yes. Basically-- Oh, go ahead.
Brigid Bergin: Go ahead as you were about to say--
Tara Haelle: I was going to say, basically when the measles outbreak happened at Disneyland, it was not the largest outbreak we had had. The largest was actually in the previous year in 2014. I think something about it happening at Disneyland, it really woke up the nation to, "Oh my gosh, this is a serious problem" because what was happening is that the measles vaccination rates were dropping in certain communities because of exemptions to school requirements. That allowed the measles to catch a foothold.
A group of parents in California decided to press for removing those exemptions so that the kids could not get exempted based on personal beliefs, they would be required to get the vaccine in order to attend school as long as they didn't have any kind of medical contraindication. There were other bills filed in other states, but the California one became the national attention-grabber. When the anti-vaccine activists tried to argue that the vaccines were dangerous, there wasn't the science there. It didn't hold weight. It didn't sway any people because we could see the danger of the measles happening and yet the evidence did not show that with the vaccines.
Then they switched tactics, and you had to call-- 2015, this was kind of the tail end of the Tea Party movement. The Tea Party was winding down. The freedom had been a big call on the right for several years now. Again, part of that distrust of government. When the anti-vaccine activists went to Conservative lawmakers and said, "Well, this is about my personal freedom. I should have the right to raise my child how I see fit. I don't want to be forced to put a pharmaceutical product in my child."
That argument actually got their attention. When they realized that that argument had their attention, that's what they started using. It's interesting because they'll often use that argument to get in the door. Then once they're in the office of the Conservative politician, they will list all the harms of vaccines, all their scientific arguments that they used to use, but they use that to get in the door. It's also they're rallying cry more broadly.
It's had a big impact because it speaks so clearly to the rhetoric that we see from the Republican Party, and it allows a lot of merging of ideas. It also kind of contributed to the, "I have a freedom not to wear a piece of cloth across my face," or "I have the freedom to go anywhere I want. You can't tell me to lockdown right now." All the different kind of presses that we see against-- different kinds of social distancing, that required testing, any kind of public health intervention, even unrelated to vaccines, has now fallen under this freedom idea and a lot of it goes back to that.
Brigid Bergin: To that moment in 2015.
Tara Haelle: Yes. I would say, there were hints of that coming before then. That just seemed to be the watershed moment when it really flipped. The push against the California law enabled the mobilization that helped them discover this together and say, "Oh, well, this really has legs. We can really use the strategy."
Brigid Bergin: In our just final few moments here, Tara, the percentage of fully vaccinated Americans right now hovers just about 50%. President Biden has made it a national priority to get those numbers up. Many are still resisting and calling out this freedom argument, choice argument, as you described. Studying this movement, what else can be done to reach these stubbornly resistant folks?
Tara Haelle: There's a lot of answers to that. We can talk for an hour on just that alone. I will say that you have to remember that there's different groups within that. There are fence-sitters and vaccine-hesitant people. There are flat-out vaccine refusers. There are anti-vaccine activists. The ones that are furthest, the absolutely most adamant refusers, you're not going to change their mind. There's always going to be a group like that. What you have to do is identify the people who do have the potential to have their mind changed, and it's going to vary.
A lot of that work, though, it's more of a one-on-one kind of work. There's not a lot of great public health top-down kinds of interventions that can address that. What can be done is teaching people how to talk to their friends and neighbors and colleagues about vaccines. There can be events that they hold at places of worship, for example, or employment centers, where they bring in a local doctor, local folks to answer questions directly and let people talk.
A lot of times, people just need an opportunity to talk to someone that they trust, who has accurate information and is not going to judge them. That sounds really basic, but we have to remember that a lot of people don't have a primary care provider in the United States. There's a lot of people who really don't have that kind of access. I think we need to create the space for that kind of access.
I think it's really something that a lot of employers, like I said, places of worship can help with, community events that can be organized by public departments of health, although they are incredibly overworked right now. It's more of an outreach kind of thing where you make a safe space for people to be able to ask questions and feel comfortable, finding out what their concerns really are.
Brigid Bergin: We're going to have to leave it there. I've been speaking with Tara Haelle, science journalist who covers vaccine hesitancy and the anti-vaccine movement, and the author of the book for young readers, Vaccination Investigation: The History and Science of Vaccines. We also spoke with Dr. Amesh Adalja, infectious disease doctor and senior scholar at the Johns Hopkins University Center for Health Security. Tara, thanks so much for coming on.
Tara Haelle: Thank you for having me.
Copyright © 2021 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.

