Ask a Virologist: What We Know (and Don't Know) About Omicron and Immunity
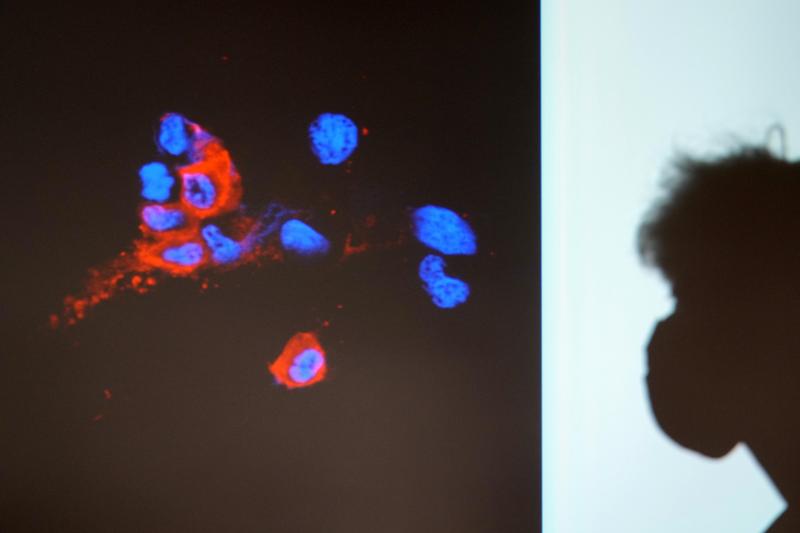
( Kin Cheung / AP Photo )
[music]
Brian Lehrer: Brian Lehrer on WNYC. It was a year ago today that Sandra Lindsay, a nurse in Queens became the first person to officially get a COVID vaccine in the United States. On that day, more than 6,000 people in New York State were hospitalized with COVID, today it's less than 4,000 hospitalized. New Jersey had 3,700 people hospitalized a year ago, now it's down to around 1,400, similar pattern in Connecticut. A year after the vaccine was introduced, the pandemic is significantly less widespread in New York, New Jersey, and Connecticut, but certainly not gone. Of course, while the vaccine has been taken by a majority of adults, it has been taken by no means at all.
In Connecticut, for example, three-quarters of the state has been fully vaccinated. Three-quarters of those hospitalized with COVID today are unvaccinated according to a report I read this week, that says a lot. More proof the vaccine is working extremely well against the worst effects of COVID even if not 100%. Now, today, on that anniversary of Sandra Lindsay's first shot in Queens, a vaccine mandate takes effect in New York City for children five and up for them to be allowed into restaurants, movie theaters, and other voluntary venues, they do not need one to go to school.
COVID cases in the tri-state area, however, are rising and that's despite just a handful infections by the new Omicron variant that had been identified so far. Connecticut, for example, had around 400 new cases a day a month ago, now it's around 2,400 new cases a day according to The New York Times COVID Tracker. Governor Hochul in New York has now restricted elective medical procedures at some upstate hospitals and ordered new vaccine or mask requirements for businesses. Governor Murphy in New Jersey and Governor Lamont in Connecticut are also sounding alarms.
A far cry, however, from the governors of Texas and Florida who are trying to ban even voluntary measures like school districts that want to have mass mandates to protect local kids or private businesses that want to have vaccine mandates on their private premises. How much at risk are we as this month of holiday gatherings continues? What do we know about Omicron and just as importantly, what don't we know yet? Is Omicron really more contagious and less virulent than the original virus as some early indications indicate?
For some insight, we're joined by Brianne Barker, an immunologist and virologist, who is an associate professor of biology at Drew University in Madison, New Jersey, and a co-host of the podcast This Week in Virology. Professor Barker, thanks so much for coming on. Welcome back to WNYC.
Dr. Brianne Barker: Thank you so much. It's great to be here, and I'm excited to answer some questions. Listeners, ask a virologist at 212-433-WNYC, 212-433-9692, or you can tweet your question @BrianLehrer. Can we start with the current rise in cases in New York, New Jersey, and Connecticut as is happening around the country? Do we know what causes these waves in case numbers, even in highly vaccinated areas like Connecticut had done so well and is now experiencing a surge compared to before?
Dr. Brianne Barker: Sure. Most of this has to do with changes in people's behavior. People who are now spending more time indoors as it's getting colder, people who are gathering with others, as you might expect near the Thanksgiving holidays, and people who are not as good with their protection with things like masks. While we have statistics that say things like 75% of individuals are being vaccinated, as you mentioned, we should remember that those statistics usually are referring to 75% of adults having been vaccinated.
We still have a large percentage of children who are not vaccinated, so if we look at our population as a whole, we're far below the proportion of people being protected that we actually need to stop the spread of this virus.
Brian Lehrer: Texas, by contrast, with only a 56% fully vaccinated rate according to The New York Times, so 20 points lower than Connecticut roughly, has seen a similar percentage drop in hospitalizations and deaths as compared to a year ago and a similar rise in new cases now, what does that stat tell us?
Dr. Brianne Barker: I think that that stat tells us that in both places, we are below the number of people we need to stop the spread of this virus. Usually, this stopping of spread, herd immunity is pretty good at really making a big change when we get to the number that we need, and that hasn't happened in either place yet.
Brian Lehrer: Yet to the effectiveness, again, 23% of the hospitalizations right now in Connecticut are fully vaccinated people, only 23% which it's about 23% of the population that's unvaccinated in Connecticut, and they make up about 75% of the cases, but I think the percentage used to be even more desperate, like only 10% of those hospitalized were vaccinated. Is there a trend in the wrong direction there?
Dr. Brianne Barker: No, that's exactly as we would expect as more and more people get vaccinated. As more people get vaccinated, we expect that, by chance, some of them will become infected. Many of those people who we see who are vaccinated and infected are what are known as incidental infections, so there are people who are being hospitalized for other reasons, and then while they are hospitalized, we are realizing that they are also positive based on infection.
Brian Lehrer: Is there recent data about where people are getting COVID? Are they bringing it home? I think the first thing most people say when I asked a question like that is people are getting it at home, it's household transmission. I'm sure that's right, but are they bringing it home? Somebody has to bring it into the house from restaurants and movie theaters, planes and trains, supermarkets, and retail stores. Are they still largely essential workers, healthcare workers, delivery workers, building service workers or not much of any of that? Is there good recent data on where people are at risk these days of getting COVID outside the home and then bringing it home for family spread?
Dr. Brianne Barker: I haven't seen good data on that recently, and data like that would be very difficult to obtain because we don't tend to see people coming up as positive until a week or so after that exposure would have happened, and it's hard to trace back over that week or so exactly where someone may have been exposed.
Brian Lehrer: Caroline in Westchester has a comparative booster question. Caroline, you're on WNYC with Dr. Brianne Barker. Hi.
Caroline: Hi. A first-time caller, a long-time listener. I have a question about mixing vaccines. My friend and I both had the two Pfizer shots. I got early, I got the Pfizer booster, she delayed, she wasn't well. She saw her doctor in between, he recommended that she get the J&J instead of the Pfizer as a third booster with her the third shot, which she did. I'm just curious, is this a good idea for people who haven't been boosted yet, and how does that relate to Omicron?
Dr. Brianne Barker: There are a couple of things here, this is a great question. If we think about the boosters in general, there is good evidence that you can mix and match the booster compared to your original vaccine dose and get an immune response that is very similar to what you would have gotten with your first dose. Some of the details of understanding vaccines might make someone want to mix and match, but the data says that all of these options are equally good, and the thing that you really want to do is get the booster that is available to you.
Based on the data that we've seen, and fortunately today, there has been some new data coming from South Africa, any of the boosters seems to do a great job at increasing your protection against Omicron. Based on the new data that came out today, boosters are very important and very effective in protection against Omicron.
Brian Lehrer: So no variability in the effectiveness of the boosters if it's not too early to tell? Moderna's giving a half dose from their originals, J&J and Pfizer the same.
Dr. Brianne Barker: No data that would really say there's any difference. It may be a little too early to tell, but based on everything that we've seen thus far, we don't see a difference based on the type of booster you get.
Brian Lehrer: I'm going to go next to Mary in White Plains who I think is going to ask a question partly about natural immunity after you've had the disease. I'm going to use that to keep a promise that I made in the last segment, which is I was going to ask you about a topic that came up from a caller in the last segment who has had COVID, says he tests positive for antibodies and doesn't think he needs a vaccine. Mary in White Plains, I'm going to let your own question in that area add to this. Mary, you're on WNYC. Hello.
Mary: Thank you. My son wanted me to find empirical evidence to show that someone like him who had COVID last November, and then who got a Johnson & Johnson vaccine in February would benefit from a booster. He's one of these people who, I'm afraid, has researched on the internet and has come up with his own answers to things, and I'm trying to convince him to get a booster and I could use some help.
Brian Lehrer: Dr. Barker.
Dr. Brianne Barker: All right, that's a great question. The trick here is that the data that I am most familiar with is data looking at vaccines other than Johnson & Johnson. Most of the data that I'm aware of on this front looks at some of the mRNA vaccines, but there is quite a bit of data showing that individuals who are infected and who then get vaccinated have exceptional levels of immunity, levels of immunity that I found incredibly impressive, and are some of the most impressive levels of immunity I've ever seen after being infected and then receiving the mRNA vaccines.
Those data refer to something called hybrid immunity and are being published from some labs in New York like the [unintelligible 00:12:03] and Bieniasz labs. Then, one could imagine because they are looking at data on infection and a vaccine that involves two doses with J&J, you would see something similar with a booster. I think it's too early for us to have data on infected individuals, and then those individuals getting both vaccinated and boosted because many of these experiments take a little bit of time, and we just haven't had enough time for the studies to have been done. Though I would expect those same groups are probably doing those experiments right now.
Brian Lehrer: Is there good science on how long immunity after having had COVID lasts compared to immunity after a vaccine? I hear you and I guess that's the top line of your answer to this question is hybrid immunity. If you've had COVID and you get vaccinated, that's like super immunity, but what about compared just one-on-one? If you've had COVID compared to if you've had the first round of vaccines, how long the immunity lasts, do we know?
Dr. Brianne Barker: We don't know exactly how long the immunity lasts, but there is a bigger issue that I think about when I'm thinking about this comparison. In those individuals who are infected only, we see a lot of variation in their immune responses. Some people, fortunately, have good immune responses, others do not, and we don't see that level of variation with the vaccine-elicited responses, people all tend to have very high responses.
If we look at some of the recent data about Omicron, for example, the data I mentioned from South Africa, they see reinfection of those who had been previously infected as being more frequent than infection of those who had been vaccinated twice. That also gives you an idea that the vaccine-elicited immunity is going to be a bit better than immunity coming from infection.
Brian Lehrer: On that note, we're going to take a short break, and then continue with immunologist and virologist, Dr. Brianne Barker, and look more closely at the evidence about Omicron. There are some dire warnings coming at least from the political sector, and I think from the medical sector in Europe now, so we'll get into the latest intelligence on Omicron with Dr. Barker and more of your calls right after this.
[music]
Brian Lehrer on WNYC as we continue with immunologist and virologist and co-host of the very esteemed, very wonky, but really compelling podcast This Week in Virology, Dr. Brianne Barker.
Dr. Barker, let's talk more about Omicron. What's different about the Omicron variant, and why are these specific differences worrisome now a few weeks after it was first identified?
Dr. Brianne Barker: One of the things that we've noticed when looking at the virus is that the virus has a surprising number of changes compared to the original virus. There are something like 30 changes in spike, which is the part of the virus targeted by vaccines, as well as changes throughout the rest of the virus. When we look at number of infections in South Africa first, we saw this virus taking over and displacing the Delta variant quite quickly. It has also taken over in the UK, in Denmark, and in Norway very quickly. This could tell us something about how transmissible the virus is, or it could tell us that those changes allow the virus to evade immune responses a little bit.
The fact that it is taking over in so many places, and some data that has started to come out in the past day or so indicate that this virus may be able to reproduce a bit better, and at least partially avoid immune responses.
Brian Lehrer: When we talk about the variant evading immunity, it sounds like a football player running down the field intentionally evading those guys trying to tackle him. Do viruses evolve with intention in that kind of way?
Dr. Brianne Barker: They do not. Viruses make mistakes when they are copying their genomes. They also sometimes can mistakenly put together different pieces of the genome that they shouldn't put together. Any particular virus that does that will be made and will attempt to reproduce. If the virus has an advantage like the ability to avoid the immune response, it will reproduce better than those viruses that did not acquire that advantage.
Brian Lehrer: Is it moving across the globe in a certain way as far as you could tell? The most dire warnings seem to be coming from the UK right now and from two Scandinavian countries in Northern Europe. Just yesterday where officials said they think Omicron is going to be, by far, the dominant variant in a matter of days, so is it geographically specific in terms of the concentration? I know there's some of it everywhere, and is that what we have to "look forward to" in this country?
Dr. Brianne Barker: I think from the data we can see now, we are likely to see quite a bit more Omicron. Omicron is going to be much more prevalent in this country. It's hard to say what kind of patterns we have in terms of spread around the world because we're limited by the amount of sequencing that's being done in different places. Right now, we know about the virus in places that are doing sequencing and looking for it, but sequencing is not done with equal frequency across the globe.
Brian Lehrer: If I'm doing the math right, and let's say it's only half as virulent than as delta, that's not known, I'm making that up, but the early indications are not as fairly virulent. Let's say it's only half as virulent as Delta but three times more spreadable, that still sounds like more hospitalizations and deaths overall, so how much of the real math of spreadable versus seriousness do you know yet?
Dr. Brianne Barker: We don't really know details on how severe this is. Some of the early data come from South Africa and there are big differences in the South African population and some of the other populations like that in the United States. They don't have as many people who are in the over 65 age group, and so we would expect to see very different patterns there. We just don't know how severe this is, but you're exactly right and it's such an important point, I'm glad you mentioned it that even if this virus is much less severe than others, the data that we have right now says it's much more transmissible and that leads to a lot more hospitalizations even if the virus is not as severe.
We need to make sure that we are supporting our health care workers by trying to prevent this virus from spreading to as many people as possible so that we can preserve hospital capacity.
Brian Lehrer: Speaking of healthcare workers, here's Elizabeth, a retired nurse in Brooklyn. Elizabeth, you're on WNYC with Dr. Barker. Hello.
Elizabeth: Hi, thank you, Dr. Barker. I'm going to try to ask this question as clearly as I can because I don't fully understand it. What I don't understand is how the immune system works. In my case, I'm not an anti-vaxer. My husband and I have been double vaxed, triple vaxed, I should say. We are in our middle and late 70s. About three weeks after my husband was triple vaxed, and I don't know if there's a connection, our doctor thinks there might be, he came down with Bell's palsy. He got Bell's palsy seven years ago, so this is now on the other side of his face. We have within our family constellation, a member who is half our age who has an autoimmune disorder.
I would like to understand what a person who has an autoimmune disorder and who has concerns about being triple-vaxed, and I do understand there's a great threat from these variants, what is happening to the immune system when you go for the next vaccine?
Dr. Brianne Barker: Sure. I will try to address your question as straightforwardly as possible. This is a topic I love to talk about.
Elizabeth: Great.
Dr. Brianne Barker: We have many different parts to your immune system. There are the antibodies and there are the T cells, but there's also a broader part of your immune system that's involved in inflammation. That happens a little earlier following the immune response. When you get that broader inflammation, and that could happen with the vaccine or that could happen with infection, you're going to generally turn on a lot of aspects of your immunity. You'll have some inflammation from the vaccine or from infection and that will turn on lots of T cells and antibodies for a little while, and they could, unfortunately, lead to that autoimmunity flare.
That person who has autoimmunity may have a little bit more inflammation on a normal day, and so getting that extra inflammation as a result of the vaccine may make them feel a little bit worse. The difficulty here is that the virus also leads to that same increase in inflammation. It, in fact, leads to a rather large and rather dysregulated form of inflammation. Unfortunately, you may have some discomfort from that third vaccine, but it's probably one might expect it might be less than you would see from getting infected. I'm definitely sorry that that happened to your husband.
Brian Lehrer: Elizabeth, good luck to you and your husband. I hope that answer was helpful in making what seems like a difficult choice. To finish up, Dr. Barker, and you've talked about age in your last couple of answers. The New York Times had a big story yesterday about COVID's toll on people over 65 where it's now the third leading cause of death. Around 1% of people over 65 in the country have been lost to COVID. That's not 1% of people who get COVID in that age group, that's 1% of the entire age group. Can you just give us a little basic science or refresher on what aging means for our immune system and why COVID is so hard on older people while some other viruses are worse for the young?
Dr. Brianne Barker: Sure. When people get older, their immune system is a little bit less able to respond to viruses. It's a little weaker perhaps is maybe the best term, I'm not quite sure there, so it is not going to respond quite as well. When individuals are younger, their immune system is going to respond in a more strong way, and so those older individuals are going to have a lot more virus. The virus is going to be able to reproduce better because it doesn't have as much of the immune system trying to stop it. As a result, you're going to have a lot of damage from the virus, and when the immune system finally does start to control the virus, the immune system is going to have to work harder.
We have a different immune response because of that hard work and a lot of virus. In younger individuals, we have a really strong immune response, sometimes that response can be a little bit in excess, and that could lead to disease in a younger individual.
Brian Lehrer: The Times says one in every hundred Americans over 65 has been lost to COVID. That compares to 1 in 1,400 people under 65. That's where we leave it for today as the pandemic continues, but so does medical science to fight the pandemic. We thank everyone who called and tweeted with your questions and we thank our guest, Brianne Barker, immunologist, and virologist who is an associate professor of biology at Drew University in Madison, New Jersey, and co-host of the podcast This Week in Virology. Thank you so much, Dr. Barker.
Dr. Brianne Barker: Thank you so much. It was great to be here.
Copyright © 2021 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.

