Tell It To Me Straight, Doc
( Dr. Brittani M. James )
Kai: This is the United States of Anxiety. A show about the unfinished business of our history and its grip on our future.
Lester Holt: Tonight, the night the world has been waiting for. The first shots given of a clinically approved COVID vaccine.
Stephanie Sierra: The closest comparison is the MMR vaccine which took start to finish four years to develop.
Kelvin Phillips: We actually have the capability, the technology to actually develop things a lot faster. I guess what I'm saying is I trust the scientists to do the right thing.
Anita Jackson: I'm going to have to convince my father because he don't know what this vaccine is about.
Bill Clinton: What was done cannot be undone but we can end the silence.
Dr. Durryle Brooks: I know testing and experimentation happened, why all of a sudden it wild for me to think that it could happen again.
Father Paul Abernathy: When we look at this COVID vaccine, it's got to be how we not only end the pandemic but how we also cure the epidemic of racial injustice in our nation.
Kai: Welcome to the show, I'm Kai Wright. Let me say right at the top, I am personally very ready to take the COVID-19 vaccine. I'm not a health worker, and I'm not particularly at risk personally, so I will have to wait some time for it, which is right and just, but when it is my turn, trust that I will be getting the shot which is a notable fact only because I am Black.
While there are lots and lots of types of people who are uneasy about the vaccine, survey data does suggest that Black Americans are uniquely worried about it, which is a problem because we are also uniquely likely to both, catch the virus, and get seriously ill from it. A lot of people are talking about this dynamic and I want to start this week's show by bringing you all into a conversation that I have been having with our associate producer, Carolyn Adams, about a viral Twitter thread she saw. Take a listen. Hey, Carolyn.
Carolyn: Hey, Kai.
Kai: This Twitter thread, you showed me a Twitter thread. What is this you're trying to get me to see?
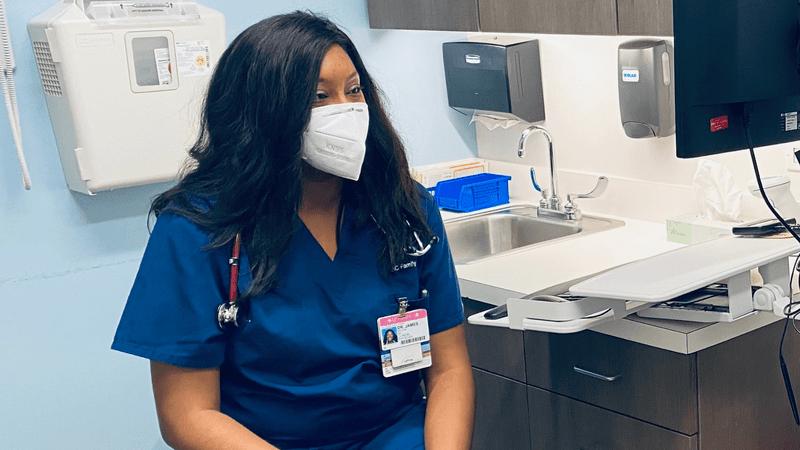
Carolyn: I found this thread on Twitter last week by Dr. Brittani James. She's a family practitioner in the southside of Chicago and the co-founder of the Institute for Antiracism in Medicine. She was addressing apprehension in the Black community. This idea that a lot of us are skeptical about taking the vaccine for pretty valid reasons.
Kai: A lot of us, meaning including you.
Carolyn: I would say it's fair to include me. I certainly am open to taking the vaccine. I'm not opposed to it. Would I be the first person in line? Probably not, but I also, like she said, understand where people are coming from.
Kai: She has this line in that Twitter thread that really hit me, too. She says, and let me quote this, "I'm a physician myself, and I even don't trust y'all. Being a doctor has made me less trusting of the medical institution as a whole, not more." There is just so much embedded in that sentence, right? Of course, it makes me think about these surveys that we've seen showing how Americans think about COVID and the vaccine, and in particular, there's the one from the Pew Center, and we can put a link to it in the show notes for this episode.
What jumped out at me is that 71% of Black people said they know somebody who is either hospitalized or killed by COVID, 71%. Then on the questions that we're sort of meant to see how seriously people are taking the pandemic, Black people were always in the lead on stuff like wearing the masks, or accepting restrictions on our behavior, right? Yet, at the same time, we were far and away the most likely to voice reluctance about taking the vaccine.
We take this thing more seriously than everyone else because we have plenty of lived experience with how dangerous it can be, and yet, we're the least likely to trust the vaccine. There are tons of reasons for that, but Dr. James' Twitter thread certainly seems to have resonated with a lot of people. Carolyn, you suggested we call Dr. James and get her to explain where she was coming from with this thread.
Dr. Brittani James: It's so interesting that that tweet went viral because I consider myself rage tweeting. Especially on matters of race, for better or worse by Twitter. Writing for me has been such an outlet for emotion and frustration. What's probably hard for people to understand is, if you're not a health care worker, to understand what's happening on the ground, for us, we feel like we're in a battle, the depth of suffering that we're around is so profound.
Then to end your day and turn on the news and people are debating about, "I don't even want to wear a mask," and on the one hand, it's great to know this vaccine is here. It gives us, the health care frontlines, a renewed sense of hope, but then, for me, it's this other pit in my stomach, knowing that history has told us, and even recent history, the way this pandemic has played out for Black and brown people, it's already predicted that this rollout is not going to be equitable. The tweet was really taking whatever ounce of power and platform I can have to say, "Let's do something about this."
Kai: I keep reading these surveys. Most recently, this Pew survey that confirms what you're saying, that there's this huge reluctance amongst Black people relative to everybody else. I keep thinking about previous epidemics, about HIV and rolling out of testing and all of it, and the times we have been reluctant to embrace health care.
Brittani: Yes, my message is that the vaccine is safe. I want people to know that. I probably said that three or four times yesterday at my clinic, too. My clinic is all Black patients, and it's already coming up. They say, "Are you going to take it?" The way they ask me, "What do you think about this, Doc?" I have this relationship with my patients, and this is something of a perk of being a Black doctor, I said, "You know, I read the study," and I'm able to say, "I'm going to do it," but I'm also saying, "I understand why you're hesitating." Because I have seated on the racism of medicine from every angle imaginable, as a Black woman, or as a physician, as a patient myself, things that I will never forget, names I was called by patients, things I overheard about Black patients or brown patients, things I've lived through.
Kai: When did that happen for you? Was it from the beginning? Were you from medical school being like, "Oh, yes, this is-- I don't trust the system"? Or was there a moment where you got to where you were like, "Oh, no, I can't trust this thing"?
Brittani: There were clues from jump. I want to be a medical professor because I thought doctors were superhuman. They're heroes, they can do no wrong, they fix people, you're saving lives, it's very romanticized, right? I saw Grey's Anatomy, Grey's Anatomy was big when I was in pre-med, like Old-school, it's been on. I remember seeing Bailey, and what Shonda Rhimes created. For me, that was my role model.
To me, when I think about that now, that was like confirmation to me, a fictional African American doctor, that maybe I can do this because I'd just never seen it. Thinking about applying to med school, I was like, what 18? You're a kid, you don't know what you're doing. You don't know what you're signing up for. I apply, it would be another what, 11, 12 years until I was done.
I'm a different person. It's still a love/hate relationship because I associate that time with a lot of trauma. Walking down the hall on the first day of med school, and seeing just the faces of all the presidents and all the classes of doctors. It's this rite of passage, this pathway that we all have to walk is lined by white men who look nothing like me. You just don't feel like you belong.
When I started taking up teaching about diseases that disproportionally hurt Black people, instead of saying Black people have higher rates of diabetes because they're more likely to live in food deserts, they're more likely to have barriers to employment that make it harder for them to maintain jobs and have a stable income, it's just taught as being Black is a risk factor for diabetes. It's subtle, but it's different because the way that we're taught was that the Black body itself inherently diseased.
Kai: Then we carry that as Black people. This was the same thing again with HIV and so many other things. Then you walk around being like, "Oh, I'm uniquely prone to disease."
Brittani: Exactly, and so I teach on antiracism in medicine and there was a long legacy of this that dates back to slavery, about the ways Black and brown bodies were made into a pathology and tested on and dehumanized. What we were taught in med school was not somehow divorced from that, but very much in the same tradition.
Carolyn: With all these disparities and problems that seem kind of baked in, do you think that the system can be changed?
Brittani: There is a huge opportunity for change, but it's not enough for a single health care provider to say, "I'm not going to be racist anymore, I'm going to treat all of my patients equally." Okay, I'm glad to hear that, but I think the thing that is so important for people to understand and think about, is that individual change is necessary, but not sufficient to lift people out of oppression.
You have to look at the policies and the structures of the bigger institutions that are creating and manufacturing the inequity. White physicians, and white health care leaders, and white administrators, they're the ones with the checkbooks, they're the ones making the actual decisions. When white people's interests and Black and brown interests converge, things are great.
When Black and brown people who equally they took an oath to protect is an afterthought. Yes, that does something to you. Such a mix of feelings, pride to be a part of the healthcare community that has the capability for great good and great innovation quickly, but shame and detachment, to also know that that is a power that is welded selectively, and not to benefit the people who need it most.
Carolyn: It's a conversation that all of us have been having with our family and our friends. The speed was something that I think crossed my mind but I'm also familiar with the amount of red tape the way funding works. I've heard about the way that AI was involved in this process. As someone who as a health care worker, you're going to be towards the front of that line. Where do you land on that yourself?
Brittani: I was raised in a similar line of thinking, what are they going to do to us, what they put in it? It's a very pervasive thing. For me what I learned is that my honest visceral reaction was nervousness when I first heard about it, it wasn't until, again, I pulled up the research myself like I wasn't going by anything anybody was telling me because of my biomedical training, I'm able to interpret it.
I'm able to link it to things that I learned, and it makes scientific sense but I understand a lot of people saying, "Oh, it is rush." Coronavirus, we've known about this family of viruses, they've been studied for over 10 years. When medicine sets their mind to something and they have money, things get done. All of a sudden, overnight, every scientist in the world was studying this particular strain, working day and night.
What feels really quick, I think is a testament to what happens when we actually have a political, moral call to action. That's really what was going on behind the scenes. To me, when I at my colleagues, they’re heroes for what they were doing. These are actually people on the other side, and these are their family members who are dying, and if it rocked the medical community, we get so lost in politics and money is that we're trying to heal people and we got to do it quick, we got to keep people safe because we took an oath.
Kai: Now, as we enter this phase, and you've got your patients on the south side, they're going to need to get vaccinated. How are you going to handle it?
Brittani: After I end this interview, I'm going to be in clinic, seeing patients you know. That's like my heartbeat. All I can do in those one on one encounters is be a friendly face in the storm, saying, "I see you, I understand your fears, you matter. I can give you the knowledge that is my best understanding of truth and understand that I have no animistic edge, I do not want to hurt you." I just use my own Black body as an example. I'm going to take it. I think that that's powerful for people.
[music]
Kai: There's a lot of water under the bridge between Black people and the nation's health care systems. The irony is that the same mistreatment and disregard for Black people that Dr. James describes also could affect the rollout of the vaccine. What do we do about that, as a society? As individuals, how do we figure out what to believe when it is simultaneously true that the health system is racist, and that we need to use it? That's next.
[music]
Welcome back. This is the United States of Anxiety. I'm Kai Wright. What's been called the most ambitious vaccine effort in American history is now underway. One COVID-19 vaccine has been approved in the US and it's being packed and shipped around the country right now. The second vaccine is expected to follow shortly. As we enter this remarkable moment together, we carry an enormous amount of history into it as individuals and as a society. Black communities in particular, but also Latinos have been far more likely to both get infected and to get seriously ill or die.
Now if surveys are correct, Black people are far more reluctant to trust the vaccines than any other group. The racism that makes us more likely to get sick, also makes us less likely to get what we need to heal. Dr. Oni Blackstock is a primary care physician in Harlem and an HIV researcher who understands this dynamic.
She's also a former Assistant Commissioner for New York City's health department where she led the city's response to the HIV epidemic. Since leaving government she's continued working on HIV as an executive director of a group called Health Justice, which consults public health organizations on racial equity. Dr. Blackstock. Hi.
Dr. Oni Blackstock: Hi, thanks so much for having me.
Kai: Thanks for coming on. I have to say you've got all those credentials, but also, who you are is an important part of this conversation. As a Black woman, you are among a disturbingly rare group of medical doctors. Dr. James we just heard from earlier she said, she told me at least that we had 2% of our doctors are Black women, that was a shocking stat to me. Had you heard that?
Blackstock: Yes, I heard. I actually have a twin sister who's also a Black woman doctor, and our mother was a Black woman doctor. In many ways actually growing up, I thought Black women doctors are really common, just given my mother's professional circle but getting further along in my training, saw that we are actually a tiny minority of physicians in this country.
Kai: Yes, you're pretty near the 2% between the three of you.
Blackstock: Exactly.
Kai: Your sister notably was on a Brian Lehrer show here on WNYC last week answering caller questions as well. Callers now Dr. Odi Blackstock is here to answer your questions. For the rest of this hour, I want to specifically hear from Black people who are worried or have heard things and want to know if their true, 646-435-7280, call us up and let's try to clear the air about the COVID vaccine.
Dr. Blackstock, so when we were listening earlier in the show to Dr. James, and she said that when she was in medical school, whenever people started talking about racial disparities in disease, something happens, where we start talking about the idea that Black people are actually uniquely prone to disease.
I feel the same thing happens when we talk about black skepticism of healthcare institutions, it suddenly sends to sound like we're saying that the blackness itself is making us crazy in some way. Why does that switch happen? Is that something that comes from public health or is that something the rest of us are putting into public health?
Blackstock: Yes, so I think that this idea of Black people as being the ones to be the pathology, or the problem lying with the individual is just part of the dominant culture. We tend to attribute behaviors and beliefs and outcomes to individuals and how they behave. Whereas I think the reality is that medical mistrust is a natural response to systemic inequity, to the way that people are treated every day living as black people in this country.
It's really a coping mechanism, and it actually can be something that can be framed in somewhat of a positive way, actually, that we do want to question, justifiably the treatments that are being recommended, vaccines that are being recommended. It's really up to these institutions, or our healthcare institutions to being the ones that are really trustworthy, that are deserving of our trust. Just trying to reframe that.
Kai: Another thing that happens is people immediately start talking about Tuskegee, and the history of the Tuskegee syphilis study. Quite honestly, most people aren't even familiar with that history, let alone the details of it. I'm wondering, in your experience, how does racist history of all sorts actually show up for individuals, for instance, with your patients, and they're making health care choices. How does the history of the country show up in those choices?
Blackstock: Right, so just to say, I do want to switch from us calling it the Tuskegee study, to its actual name, which is the US public health service, syphilis study at Tuskegee, because as you know, Tuskegee is a historically Black university. It was the site of the study, but the US government was the one that carried out the actual study.
The reality is, some of my patients who are older, they are aware of Tuskegee but a lot of my younger patients aren't. They do know just how they're treated when they come to, for instance, a clinic. They've had other health care providers treat them in ways that were very disrespectful, where they made assumptions about what the patient understood.
It's just the everyday treatment either within the healthcare setting and just like being out in the world as a Black person, that really affects the level of trust that many Black people have in health care providers, and just to say, people often will trust their individual health care provider but may have larger issues around mistrust of the actual sort of healthcare system or to health care enterprise, government largely, pharma. We see that happening often.
Just to say that individual providers can actually make a big difference in raising the discussion of the vaccine with our patients, and really asking what they know, and asking permission to share information with the
patient to correct any misunderstandings or misconceptions that the patient has.
Kai: Speaking of things that worked, you have a significant history in working on HIV, as I said earlier. There's lots of lessons I imagine there when we think about misinformation in the Black community with how it spreads, and how it gets fixed. Let's start with the former certainly by the late 1990s, HIV had become a uniquely Black epidemic all over the planet and remain so today.
There was so much skepticism about public health and misinformation about the virus out there. Speaking about how that problem happened, how did that come to be at that time? Can we use that specific epidemic as a way to explain how history of racism and abuse shows up when public health tries to communicate with Black people?
Blackstock: Right, I think similar to COVID-19, where we saw this very delayed and really grossly inadequate government response to the pandemic. We saw something very similar with the HIV epidemic with President Reagan, who was in leadership at the time, took as much as four years to actually say the word AIDS. By that time, more than 10,000 Americans had died from HIV, so there was government silence, there was government inaction.
I think all of that also contributes to the lack of trust that folks have. We saw this similarly, with COVID-19, as well a lack of appropriate response, a national response, a coordinated response to this pandemic. What that does is, when there is an action, when there's a lack of transparency, people create their own narratives, they create their own stories.
Something like HIV, which was a newer virus as compared to measles or mumps, people because of the way that they were treated and marginalized by society develop their own narratives about HIV possibly being manmade, HIV being created to kill off Black people. HIV treatment not being a treatment but instead a poison for Black people. These are all-- I don't actually call them conspiracy beliefs, I call them counter-narratives because they're not unreasonable. It's not unreasonable.
It's so important to validate and be like, "I understand that you would have these concerns, and we've also seen people live very long, healthy lives with HIV treatment." It's like holding space for these counter-narratives and these beliefs that may be different from the beliefs of the dominant culture, and also saying, "Look, we also have all of this data to show that these treatments are safe and effective and I will, as your provider work with you if you have any questions or concerns."
Kai: Holding space for both and. We struggled so hard in our culture to do both and. an American culture, we're so invested in either or so I appreciate that perspective. Let's hear from Deborah in Montclair, New Jersey. Deborah, welcome to the show. Do you have a question for Dr. Blackstock?
Deborah: Thank you very much, and good evening to you, Kai, and also to your guests. What my concern is that normally, pharmaceuticals will take years to develop a medication, where I understand this is a pandemic and it's very, very serious. I worry about the fact that normally it's-- As I said, it takes them years and years to develop something. Now all of a sudden, within a few months, they're capable of doing it. If you can do it now for this, why can't they do it for any other illness? It's just to me they did this so fast that it worries me.
Kai: Debra's question, Debra, so many people have this question. I feel like it's the most common thing I heard. My mother asked it to me. I have friends who asked it to me. Dr. Blackstock, how do we wrap our head around that?
Blackstock: Right now I think that is a totally valid concern. Yes, the speed at which this vaccine was developed and authorized is a record. I think the reason why, and I think Dr. James spoke to this as well. There was no political will, there were hundreds of millions of dollars that were basically-- that went from the government to these pharmaceutical companies. The government paid for these phase three clinical trials, the trials looking at safety and efficacy, and also paid for the mass production.
You would have never seen a pharmaceutical company, be willing to make this investment upfront. Also what's important is that instead of having each step of the vaccine development and testing process happen sequentially like one after another, many of these processes happened in parallel in order to expedite the process. No steps actually were missed or bypassed. Everything was done. It was done just as rigorously, but in a compressed timeline, because many steps were performed in parallel.
I think it's just important for folks to understand like, yes, I think because COVID-19 affects everybody, obviously, it has a disproportionate impact on Black folk and other people of color. I think because it affects everyone, there was an investment, there was political will to make the financial investment necessary to get this done in record time.
Kai: Seeing that and it's this is where the rubber hits the road, because on one hand, you're like, "Okay, great." Then to hear that last piece, oh, right, so maybe we could have had an HIV vaccine by now, or maybe we could have had treatments for other things that are they're uniquely impacting African Americans. That leads to this distrust.
Blackstock: Totally. I have had conversations with my patients who are living with HIV because the reality is pharmaceutical companies that are making HIV treatment, they basically have patients or customers for life because people with HIV, ideally, you'd be taking HIV medication for decades. I've had patients say, "Well, why would they develop a vaccine when they could have be paying for HIV treatment for decades and make so much more money off of that as opposed to eradicating HIV?"
It does raise a lot of questions. I think the reality is HIV disproportionately impacts people of color, not just here in the United States, but in Sub-Saharan Africa, in Asia and there's not the same will on part of the pharmaceutical companies, government to develop a vaccine in the same record time.
Kai: The bottom line answer to Deborah's question, because they spent a lot of money and were able to do it faster and that helps. Let's go to Stephen in Highland Falls. Steven, welcome to the show.
Stephen: Welcome to y'all and blessings to y'all.
Kai: Blessings to you. Do you have a question for Dr. Blackstock?
Stephen: Yes. Thank you. I'm a 61-year-old person of color. I actually had a COVID-19 and had a pretty severe within early April to early May. My question would be, and I'm still hesitant about taking the vaccine and for the sake of clarity, I was wondering how come there isn't an agenda to put it in layman's terms so that the common person actually knows what's actually in it? You know what I mean? I think the unknown is why people have a lot of hesitancy like what's in it.
Kai: How about that?
Blackstock: Yes. Just to say, I'm so glad that you were able to recover and that you are here with us? Yes, I think that we need to do a much better job as a "public health system." I say, quote, unquote, because we don't actually have a public health system, a coordinated system, but to really educate people about how the vaccine works. Hopefully, we will see mass public health campaigns that describe how it works.
Basically, I can just say very quickly, the way the vaccine works is that the mRNA gives instructions to the muscle cells to basically make this spike protein that's found on the novel Coronavirus. Then once the body starts producing the spike protein, the body launches an immune response to that protein.
Now that your body has seen the spike protein, which this protein that the body makes is a harmless protein, but it resembles the one that's actually on the virus. When you're actually exposed, your body has the memory of seeing that spike protein, and the antibodies and white blood cells are then ready and poised to attack the virus if you are infected.
Kai: This is a new kind of vaccine, right? This is the other thing, I feel like people are trying to wrap their heads around. You're not actually being injected with a virus, you're being injected with something that will teach your body to respond to the virus and that's a new technology.
Blackstock: There has been, I guess, a number of years of study of mRNA vaccines for other infectious diseases. This is the first time though that mRNA vaccine has gotten this far along to show safety and efficacy and have been either authorized or approved for use. The concept is one that has been studied for a great deal of time. It's just that this is the first approved or authorized vaccine that uses this technology.
Just to say it includes so something called Adjaven which is extra ingredient that helps to stimulate a stronger immune response. It also has salts and sugars and lipids, also known as fat. A lot of things that are actually found naturally in the body are in the vaccine, in addition, to obviously the mRNA that gives the instructions to the body.
Kai: Stephen, I hope that helps. Let's go to Damani in Brooklyn. Damani, welcome to the show.
Damani: Hi, thank you so much for having me. My concern is with the side effects. Most of the reason why I choose not to take pharmaceuticals and go the medicinal route is because normally, there are side effects that will then cause me to have to take another pharmaceutical for that side effects and so forth and so on. Can you address what we can expect in the side effects of taking this vaccine?
Blackstock: Sure, yes. Side effects, obviously, I think are a concern to most folks. In the clinical trials that have been done, basically, the Pfizer trial, the most common side effect was some pain or discomfort at the site where the participant had the injection. Then folks also had headaches, fatigue, muscle pain, and fever but these were typically mild to moderate and very short-lived, lasting one to two days.
I think what's really important for folks to understand is that all of these symptoms, for the most part, fever, headache, muscle pain, fatigue, all of these are basically a result of the body responding to the vaccine, it's the body developing it's an immune response. Actually, it's a good thing. It actually means that your body is now working hard in response to the vaccine that you receive. A lot of times, we don't really say this is a side effect, we say it's like a reaction to the vaccine in a very normal and natural reaction.
[music]
Kai: This is the United States of Anxiety, and I'm Kai Wright we'll take more of your calls after a break.
[music]
Hey, this is Kai. Just a quick program note here. When we started making this show back in 2016, we were just trying to bring context to that wild campaign season, and particularly the history that we all carried into it. Initially, we figured we'd stop after that election but obviously, there was a lot more to chew on which is just to say, if you're new to the show, there are tons of episodes here that I hope you'll check out. We've taken snapshots of the political culture.
Speaker 8: It's not right, I'm sorry. I feel bad for people that are oppressed, and I mean oppressed but if we can take care of our own too.
Kai: We've asked how power is really built in a democracy.
Speaker 9: I don't believe the demography is destiny. I think demography is a pathway but it takes work. We're the first campaign in the deep south to put in the work.
Kai: We've just mined all kinds of history in an effort to put America on the couch, to understand how we got here as a country, and where we're going. I urge you to dig around in the archives. It is all still relevant. If you hear something that raises new questions for you, and you want us to follow up on that, hit me up, email me at anxiety@wnyc.org and maybe we'll take you up on it. Thanks so much.
[music]
Dr. Blackstock, I have to admit that I only just learned that the lead scientist for the vaccine research at the National Institutes of Health is a Black woman her name is Dr. Kizzy Corbett. Anthony Fauci made special note of her role the other day, and she is the top scientist behind the Moderna vaccine, which is likely to be the next one approved. I just want to play something. Here's something she said on the CNN podcast Coronavirus: Fact Versus Fiction. It's about a minute long.
Kizzy: We're not going to be able to prove trustworthiness, in this instance quickly and that is okay. What we do need to do is decide that we're going to take steps and even beyond this pandemic move in the direction to be more trustworthy. The reason why I say we, and the reason why I say trustworthy, instead of using the terminology they or distrust is because the first step is that as scientists and physicians and vaccine developers and et cetera, is to understand that the onus of this problem is not on them and their distrust. It is on us and our level of trustworthiness.
Kai: That's Dr. Kizzy Corbett, who is the head of vaccine research at the National Institutes of Health, sharp words from her. Dr. Blackstock do you know, Dr. Corbett and do you think it's important that she's in this role as a Black woman? Do you think that matters in this conversation we're having?
Blackstock: Oh, it's totally important. I don't personally know Dr. Corbett, but I know myself and many other Black women doctors are cheering her from the sidelines. I think it's incredibly important that she's in the position she's in and I think people can look to her, they can see someone who looks like their daughter, their niece, their cousin, and someone who is intimately involved with the work, very knowledgeable about it, and who can be a potentially really trusted messenger to many in the Black community.
Kai: Let's go to Mayet in Bed-Stuy. Mayet, welcome to the show.
Mayet: Yes, I'm not in Bed-Stuy but thanks for taking my call.
Kai: Oh my apologies.
Mayet: I have three points, I'll make briefly and I'd like the response to. First of all, Dr. William Haseltine, formerly of Harvard, very renowned, he spoke to the fact that 20% of a population cannot take a vaccine he specifically mentioned elders who need to have a much higher ramped up dose, because of the body doesn't recognize the dose. He mentioned HIV, MERS, SARS, nothing vaccine wise in those areas.
The second point has to deal with look at the rest of the world over 100 years ago after the flu pandemic, many nations brought in universal health care. Canada gives 2,000 a month during the pandemic so if people are sick, they can stay home, and they have some foundation. That's a big area of distrust. The last point has to do with another community station at five this morning in other news brought forth [doctor], a history Royal Raymond Rice who invented a microscope that fluoresces viruses.
He also came up with a machine around frequencies, the medical establishment, when we need another approach, suppressed it, oppress it. I think he wound up in jail but this seems to be a branch of medicine that I'd like to know if they're familiar with as electronic energy medicine and whether this should be looked at in a more fairway. I'll listen over the air for the response. Thank you.
Kai: Thank you, Mayet. Now. There are three long questions there, Dr. Blackstock, are you able to answer any of them?
Blackstock: Yes, just to my first point around older folks may be needing a higher dose, that may be needed in the future, we'll look at the data and see perhaps if there is a booster dose that's needed. As of now, it looks like regardless of age, the Pfizer vaccine, at least, was protective against COVID-19 or becoming having symptoms of COVID-19 but there is a concern, obviously, for that older folks sometimes do not generate as vigorous or robust an immune response.
I think as time goes on, we will figure out is there one vaccine, in particular, that's better for older folks or is there a booster that's needed? To our second point around universal health care. Yes, yes, yes, I think the fact of the fact that I actually tweeted this, just yesterday. The fact that there are still states in the United States that have not, for instance, expanded Medicaid. We haven't talked about universal health care, just Medicaid expansion, in the middle of a pandemic it's criminal, and almost a human rights violation, to be honest.
Universal health care would be incredibly important to institute and I think I know myself and other advocates, this is something that we have been pushing for and will continue to push for with the new federal administration. Then the last question, I actually don't know about electronic energy medicines but as far as COVID-19, and various treatments and vaccines, just know that there are many different technologies and platforms that are being studied. I think within the next year, we're going to see many more options available.
Kai: That's very impressive, Dr. Blackstock you got through all of this. Thank you for that. Let's get to Bailey in the Bronx. Bailey, welcome to the show.
Bailey: Oh, thank you. How are you?
Kai: Very
well, do you have a question for Dr. Blackstock?
Bailey: Actually, I'm in the Johnson & Johnson third phase. I just took the shot on Friday.
Kai: Oh, what is your experience been like?
Bailey: I don't know. I think they gave me the placebo because I have more energy than I've ever had before. Honestly, I was like, "Wow, I really feel good," but it wasn't bad. They asked a lot of questions. It's through the VA. They're trying to get 100 people by Thursday. Vets are like, "No." They will not do it because we get experimented on a lot.
It's really funny because this is a little distrust of the government, the present government. When Putin said he had and I was like, "Oh, my God, they're going to be using it," the Russian vaccine on vets in the military. When I went to the place, the woman was Russian who took the survey. I was like, "Oh, my God, I'm telling the truth," but when they explained everything, it was fine.
Kai: What made you volunteer?
Bailey: I know that they don't have enough minorities in studies for pharmaceuticals, anyway. When I was looking at the early participants in the vaccine, they were always white that I was seeing on the news, which I thought was really weird because it was affecting the minority population the most. When I found out the VA was opening up a study, I took advantage of it.
Kai: Thank you, Bailey, for calling in and sharing that with us. What do you think about any of that, Dr. Blackstock? Particularly this question of having to get more Black, because we still need-- the trials are ongoing, right? They still have this problem with having not enough people of color enrolled.
Blackstock: Yes. Thank you to Bailey for her decision to participate in the Johnson & Johnson study. It's very brave of her and I think many of us are very grateful for her service. Yes, it's a huge issue. I think obviously, this issue around mistrust and just like, everyday racism impacts Black people's desire to be in clinical trials and to be tested on just given the centuries of medical experimentation that is part of our legacy in this country. It's incredibly important that Black folk and other people of color, be part of these clinical trials.
Number one, knowing that Black people were involved, Latino people, it can help to build trust in research and the research enterprise. Also, it's important to know, how did these vaccines affect us differently? Not because there are any differences in genetically between Black people and other groups of people, but because our lived experiences the effects of racism, the weathering effect that it has on us. How could that have some impact on the way that the vaccine protects us or does it protect us, or does it protect us? All of that's important. I think it's great that Bailey is part of the study and definitely encouraging more folks to enroll if they have an interest.
Kai: Another question on the studies on the ongoing trials is caller, who did not want to be on the air, but wanted to know, how do we trust the long term of the side effects when there's only three months worth of data so far?
Blackstock: Right. Yes. All of these pharmaceutical companies are going to be continuing to collect data. Again, many of the studies are ongoing so they're going to continue to collect safety data. There's also data that's going to be collected post-marketing. There is the vaccine adverse events reporting system. That's, I believe, run by the CDC, where physicians, other health care providers can report vaccine side effects.
Then also, there's going to be-- I think that's not CDC run, but V-safe, I believe, will be an app that the CDC is putting out when someone gets the vaccine, they can then report any adverse effects they have. That all of this data is going to be collected and looked at in a rigorous way, in a systematic way, so that if there are any concerning signals, those can be identified and addressed.
Kai: I think we have time to get one more caller and at least let's go to Don in Manistee, Michigan. Don, welcome to the show.
Don: Thank you, Dr. Blackstock. I'd like to express that I understand that this is a human condition. This virus that attacked is something from out of space. As a human family, we have to get together to kill this out of space being. How do we explain to people that the science tells us that this vaccine works?
As far as trials go, I understand scientific methods and trials, et cetera but as far as trials go in regards to Black and brown people, we're the ones who are on the frontlines. We are the ones who have been exposed to the virus, a living trial. If there's something happened, there are most of us who are dying than anybody else?
Blackstock: Yes, I want to acknowledge that. Yes, we are being heavily impacted. I appreciate your point about this being a living trial. What I am happy to do with my patients and I think that we need to do on a larger level is really explained like, how these studies happen. That certain participants will get the actual investigative vaccine, others will get sort of a placebo vaccine or one that does not have the investigational vaccine. Understand how people are followed, what data is collected?
I think that we can explain this in a way that is very clear to people and understandable but I think that we have not gotten to that point yet. In addition to explaining the safety of the vaccine, we need to understand well, how is it studied? I agree, I think it's up to healthcare providers, the health care system, public health to make sure that patients and those out in the community are as informed as possible so that they can make the best decision possible for themselves about whether to get the vaccine or not?
Kai: Dr. Oni Blackstock is a primary care physician in Harlem and an HIV researcher. She's a former Assistant Commissioner in New York City's health department, where she led the city's response to HIV. She continues working on HIV as executive director of Health Justice, an organization that consults with public health organizations on racial equity. Dr. Blackstock, thank you so much for taking this time.
Blackstock: You're very welcome
[music]
Kai: United States of Anxiety is a production of WNYC Studios. Jared Paul mixed the podcast version. Kevin Bristow and Matthew Marando, were at the board's for the live show. Our team also includes Carolyn Adams and Emily Botein, Jenny Casas, Marianne McCune, Christopher Werth and Veralyn Williams. A theme music was written by Hannis Brown and performed by the Outer Borough Brass Band.
Karen Frillmann is our executive producer and I am Kai Wright. You can keep in touch with me on Twitter @kai_wright. That's Wright like the brothers. As always, I hope you'll join us for the live show every Sunday 6:00 PM, Eastern. Stream it at wnyc.org or tell your smart speaker play WNYC. Till then, thanks for listening. Take care of yourselves and happy holidays.
[music]
Copyright © 2020 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.