ACT UP, Fight Covid
Kai: This is the United States of Anxiety, a show about the unfinished business of our history and its grip on our future.
Reporter 1: This morning, the most vulnerable Americans. Now, one step closer to getting a COVID vaccine.
Testing Site Nurse: We’re going to do a nasal swab. So it is going to go back. It’s going to be uncomfortable.
Eli Vazquez: All these things that you're hearing about in the news is frustrating, but it hits different when you're going through it.
Reporter 2: The confusion and anxiety many are feeling has drawn parallels to the HIV/AIDS epidemic of the 1980s.
Ken Williams: Transparency has always been my currency. Why couldn't I tell my mother I had HIV?
Phil Wilson: Our friends were getting sick and our friends were dying. If you were a person of conscience you had to get involved.
Protester: The main reason I'm here to scatter my own ashes, I'm going to die of AIDS in probably two years.
Zoe Leonard: What AIDS revealed was not the problem of the virus. What AIDS revealed is the problems of our society.
Kai: Welcome to the show. I'm Kai Wright. Last week I was sitting in a clinic waiting for results from a rapid COVID test when I had this vivid flash of memory. I was snatched back to being a young gay man sitting in an HIV clinic in the mid-1990s, waiting for test results because that was a new routine back then, going in for regular HIV tests, waiting for the results.
For me, at least, no matter what actual risks I'd taken, always, always feeling dread because it was so fraught. It was about so much more than physical health. HIV has been a constant intimate companion my whole adult life. If you're someone who came of sexual age in the '80s and '90s, especially if you're gay or transgender, then there's a good chance HIV has occupied a lot of space in your mind and heart as well. Whether we're positive or negative, it doesn't matter, the virus has just been present.
When COVID-19 crashed our lives back in February, a lot of people immediately began thinking about those early pretreatment days of HIV, from a public health perspective, from a political perspective certainly, but also it triggered something in our emotional memories. We're going to spend this week's show in that space, reminding ourselves of the history of treatment activism in particular around HIV and trying to apply lessons from that history to COVID.
We've just had World AIDS Day. Next summer, we'll mark 40 maddening years since the CDC first reported on the virus. HIV has killed tens of millions of people since that report, 38 million people continue to live with it today. Thankfully, there are now treatments that make it livable though they are still not universally accessible. As with COVID, New York City was one of the first places in the US to be overwhelmed by HIV.
Our executive producer, Karen Frillmann was a young woman in the city at the time and when COVID hit here, Karen found herself rustling around in her closet, digging out a recording she made 34 years when there was still so much we didn't know about HIV. We've asked her to open that time capsule for us and she begins by just remembering how it all started for her.
Karen: I volunteered for a small agency to go in, to clean, and to bring food. I remember going and meeting this young man, his name was John. When I first started to care for him, I felt like I was taking care of someone my brother's age, and then within a few weeks, this young man aged right before my eyes and he was gone in three-and-a-half months. It is so frightening to see life just slip away.
Kai: It reminds me of particularly the spring when we were hearing and people would go to the hospital, and within it so quickly people would go from not feeling well to not being able to breathe to being gone.
Karen: Yes, that's right. At that time it was happening to these young, vibrant people who were just really bringing so much to New York City. After that, I decided to begin to record people and to basically start to document some of what I was seeing. [crosstalk] I met Michael Calvert through a friend of a friend.
Michael: Did y'all get specific questions that you want to ask me-
Karen: It was July of 1986 and he invited me up to his apartment.
Judy Wenning: Maybe we should mark him with a regular marker.
Karen: Judy Wenning, who was my producing partner at the time.
Judy: How have you been feeling?
Michael: I've been feeling rotten. It's the truth.
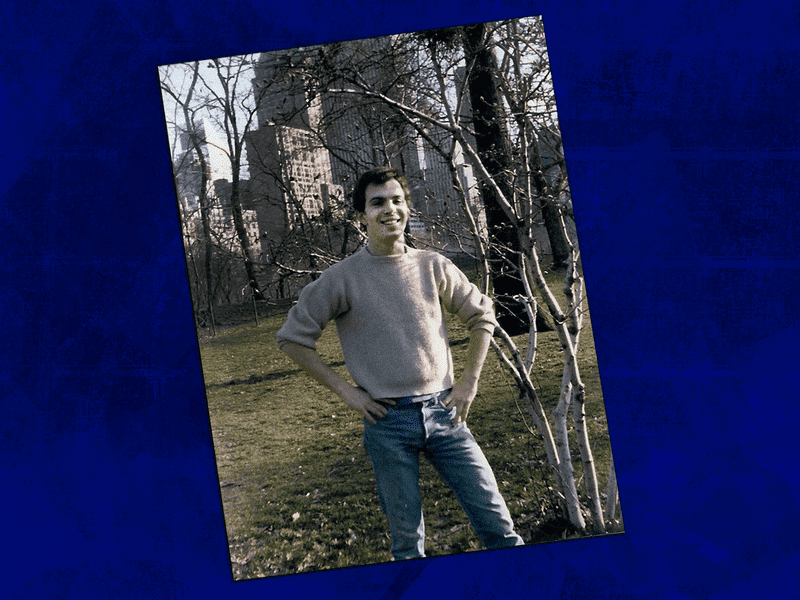
Karen: He was 27 years old when I met him. He was living in Chelsea.
Michael: I don't really know why, but just rotten and I think maybe it's been as mentally a problem as it has physically, the physical pain and the-
Karen: At that time, I think the thing that was really grounding him, he was a member of the People With AIDS Coalition, which was an advocacy group and a support group for these people who were getting sick. There was so much of a stigma around it. People didn't understand it. Michael had started giving talks, educating healthcare workers about what this disease was doing.
Michael: I showed people my lesions today, a spot that I don't even look at on a regular basis. I don't want to see them. I put on a long sleeve shirt so that I don't see them not so that other people can't. It was really odd today for me to uncover them for myself in order to show them to other people.
Karen: Michael was a little self-conscious about what AIDS had done to his appearance.
Judy: How did that feel?
Michael: I wanted to ask questions about it and that was okay. It didn't bother me a bit.
Michael: He was still very cute, and slight build, very thin and he was Southern. He'd moved to New York when he was 20 years old. That's the thing. He was young.
Michael: I can show you a beautiful picture of me at age 20.
Judy: I like your hair long.
Michael: I like my hair long too.
Karen: He'd come from Gadsden, Alabama, where he'd been a straight-A student.
Michael: I smoked pot after school with the kids and told them what to study so they can make passing grades.
Karen: He'd started acting in local theater and I think he'd been a star in his town.
Michael: I never had a pimple and then went to the theater every afternoon evening and had this whole other group of friends, wild, mystical, free-spirited type friends, and Matt Oliver things.
Judy: You didn't live at home?
Michael: I did live at home and I kept my curfew all those nights. Because I was smart because I was honest, my curfew was one o'clock. They'd rather me be home before that, but they knew I was in the theater. I was in the newspaper every six weeks so it wasn't like they didn't trust me.
Judy: They also knew you were in a relationship.
Michael: They didn't know I was in a relationship with this man.
Karen: When Michael came to New York, that's what he wanted to do. He wanted to be an actor and he talks about that moment in New York City as being totally life-changing for him.
Michael: I was wild and it was wonderful, and I was not afraid to experience anything and everything when I first came to New York, but I wasn't disciplined. I didn't get what I really came here for as far as acting. I allowed the discovery part of my life to take over and just to do what I wanted to do.
Karen: To support himself, Michael had developed a flower business, which you would be walking down a street in the West Village and these little outrageously beautiful flower shops had appeared, it was orchids and bird of paradise, stuff that just, in New York City at that time, which was pretty run down, it was just a gorgeous contrast.
Rick: The sad part is-- there are so many sad parts, but the flower design business was just taking off. By taking off, I mean he was getting some big clients and it was becoming finally lucrative.
Kai: That's Rick Kitzman. Karen, I got to say, I'm really glad you invited me to join you when you met him because having heard all these recordings of Michael from three decades ago, I was really longing to meet somebody who was close to him.
Karen: Rick came to New York City in the late '70s from Colorado. They met through mutual friends and started dating.
Rick: When you said, "We want to ask about Michael Calvert," when I read that bam, all of these emotions just came. It was so out of the blue and I was just overcome for five seconds of all these thoughts, feelings, and emotions just thinking about Michael Calvert that came up from the time.
Karen: Can you tell us a little bit about him? how you knew him?
Rick: It was about '83, '84, my roommate Sarah Myers and I threw a party called The Well-Red Party so not only did everybody wear red, but it was also about reading books. It was one of those clever, witty New York things you did in the '80s. Michael came and we just hit it off. He was adorably cute and he was funnier than hell. I grew to just love that Southern charm.
I remember The Well-Red Party, we invited practically everybody we knew and Michael did the flowers. What I remember, so distinctly was he brought as many red flowers as he could find and so that little apartment was just covered with bouquets of red flowers. We wanted a boutonnière for me and we wanted a corsage for Sarah. There's no such thing as a red orchid, the closest is a deep orange and so that was her corsage.
He was done putting up all the flowers and I'm going, "Well, what about me? Where's my boutonnière?" He said, "Oh, I didn't forget you." He took it an anthurium and those are those-- well, we call them the little boy flowers because they have blood-red more or less leaves with a statement of about an inch-and-a-half long of bright gold, yellow. He took one of those, he cut it into a triangle and pinned it to my shirt and that was my corsage. I just thought it was so amazingly creative.
Michael and I, we just had a good time with each other and the flip side was, it became really a time of grief and fear and eventually rage. This friend got sick. I would hear about this friend who got sick and the situation for me became just untenable. It was in '85 that I decided I just had to leave New York because I knew something really bad was going to happen to me.
I remember the last time I-- I'm almost positive, it's the last time I saw Michael and I think he was taking me to LaGuardia. We were in his van and the back was filled with flowers. As I recall, he wished I would stay, but he understood. I remember he talked about this client and that client and this party and that party. You could tell there was this joy of what he was doing because he found something, it may not have been the reason he moved to New York, but that he loved doing and that he was becoming successful doing.
For Michael, that was a new achievement. It was just really fun to be a part of that and to hear his enthusiasm contrasted with the sadness of leaving each other. I think part of that sadness was, on some level, it's possible we knew that we wouldn't see each other again.
[music]
Michael: Is the tape going? Because I want to say this. I did have a good time when I first came to New York and I'm still having a good time. I really love my life and I think that that makes me a special person because I don't think there are a lot of people in this world that do. The good times have not stopped just because I hurt and it's really important for me to try to share that with people and to try to help them understand that you can get through difficulty, and still have a wonderful, beautiful life.
Kai: What did ultimately happen with Michael and his health?
Karen: Judy and I met Michael about a year after he was diagnosed. He had had a little bit of time to come to terms with what was happening to him, but he was getting weaker and I think sicker.
Michael: The main problem is just the pain. I try to describe it in therapy. This is more like heartache pain. That kind of pain. Pain that's all over, that's indescribable. You can't put your finger on it. It just hurts all over.
Karen: I think you can hear in his voice, the mental anguish that he was experiencing
Michael: I dealt with feelings of giving up, wondering where my hope was, wondering if I was going to stay that way, not believing that I could possibly stay that way because it was miserable. It would turn in from two days in misery to three to a week and then I thought, "My God, how am I going to go on this way? I absolutely can't." I'm wondering, "is it going to be another week or months or the rest of my life?" Not believing that it could be the rest of my life, but wondering was a major step, a major thing for me because I never wondered in my life about going on.
Karen: You've never felt hopeless before then?
Michael: Not really.
Karen: Another really terrible thing about that time was that some of these young men were shunned by their families. Their parents cut them off. They wouldn't talk to them. You told your mother on the phone?
Michael: I told my mother on the phone. I had to call her at work. She didn't have a phone.
Karen: Michael actually had a good relationship with his parents and his siblings.
Michael: My father was the most upset.
Karen: I think he was touched by how accepting and supportive they were.
Michael: They loved me anyway, without any question, without any hesitation. I think that meant more than anything. They didn't have to say it, I can tell. I was there. I was with him and should have told them. The telephone doesn't keep people apart. It doesn't separate people and it really brings people together. I think that even though it was on the phone that I told my mother, she loved me anyway.
Karen: Your family really cares about yourself.
Michael: Oh yes. I'm very, very lucky in that sense. They're not hiding away. I think they're struggling to stay away as much as I want them to.
Karen: He wanted to be independent. He wanted to continue to take care of himself and live his life. I'd hear how much he was struggling with the idea of his decline.
Michael: The mean people poke and prod, especially mentally, not necessarily physically, but, "They want to know. How can I help you? I'll do anything. You just call me. Just call me. Whose need is that? It ain't mine."
Karen: You want to stay independent how long?
Michael: Forever, just like you. I would think everybody wants to be free and I don't want to be dependent. I don't want to be dependent on anyone. You know what? I'm liable to die before I get the chance to express a lot of what's inside of me.
Karen: You know, he was 27 years old. He was really just trying to maintain his equilibrium.
Kai: I've thought about this a lot too, as a gay man who came of age just after Michael's generation is a lot of men his age, they're almost like first-generation that show up in a place like New York and San Francisco and Washington D.C. from wherever they had come and they had to do so much to create their lives in those places. They literally created the gay world in which I now live. They made space for themselves and they were just getting that space. It was just coming into fruition, and just when he's got it to be faced with something like this.
Michael: [coughs] I'm not crazy about the fact that I have AIDS. It's difficult and it's a real burden. It's a burden because there's a certain responsibility to helping other people through it because it's such a difficult thing. It's a burden because it hurts. I also don't think that this isn't necessarily going to kill me before my time. It may and it may not. I'm doing everything I can so that it doesn't, that's part of the burden.
Karen: When I met him in '86, he swung between feeling very down to believing that he was going to be a survivor, and of course there was a quest at that time to find a cure.
Michael: I, fortunately, don't think that I'm to be in captivity forever. There's probably something on the way. I still feel like I'll beat the odds. They say, "18 months", I say, "19", they say, "20" and I say, "Oh, 24." I don't care what they say. I know how I feel. It's been a year and I feel like I got at least another good year in me and by that time, something should happen that'll help me get through another year, by that time a cure and by that time, by that time, by that time. That's how I really think. That's how I really, really, really think. Is that denial? Is that stupid? Is that not recognizing the reality? No, because I do know the reality.
Kai: I just hear such confidence and optimism in the face of this diagnosis, in the face of this disease that I now know would kill so many people.
Michael: Whatever's statistics you quote, I'm going to beat. I'm going to be the person that changes those statistics. Let me tell you that right now. No way am I just living at 18 more months.
Karen: One of the things that taking this tape, listening to it 34 years later, it's partly just the act of remembering and the act of saying that this man walked the streets and contributed to the life of our city. Michael died about five months after we recorded him. He died too young, but that's something we can do is remember.
Kai: At a time when we've buried 207,000 people?
Karen: Yes. We’re just about out of tape, and all I want you to do is just be quiet for a moment till it runs out.
Michael: Oh.
[sound cut]
[music]
Kai: Welcome back. This is the United States of Anxiety and I'm Kai Wright. This week, we are asking what we can learn from nearly 40 years of the HIV/AIDS pandemic as we approach one year of living with COVID-19. Both pandemics hit the New York area with particular fury at their outset and so for the rest of this show, I want to invite you to call in with your own memories of the early HIV epidemic.
As we take your calls, I'm joined by somebody who was here fighting to save lives in his community, which is now my community, and who has also been thinking a great deal about our response to COVID-19. Gregg Gonsalves was a founder of the Treatment Action Group in 1992, which grew out of ACT UP and he has never stopped being an AIDS activist. He's also now an epidemiologist and co-director of the Global Health Justice Partnership at Yale University. He's been writing about our national response to COVID for The Nation Magazine. Gregg, thanks for joining us.
Gregg: Anytime Kai, thanks for having me.
Kai: Gregg, I'd like to start with some of your own early memories of the HIV epidemic here in New York. I know you grew up here in Long Island. You went off to college, but you came home to New York in 1990, and by that time you were already a member of ACT UP. I gather your own activism was at least partly driven by your effort to just keep your boyfriend alive at the time.
We just heard Michael Calvert, that young man wondering aloud back in 1986, it was about, whether science would catch up in time to save his life. Do you recall how you guys felt at that time, not only waiting for science to catch up but also fighting to make it happen? What was that like for you guys?
Gregg: It just was unbearable, frankly. Just hearing those voices over the past half-hour on your show was just incredibly painful because I remember being enacted at meetings on Monday nights, people coming up to me and talking to me about cryptosporidiosis, which was diseases that Treatment and Data Committee of ACT UP had assigned to me when I first got there, asking about new treatments, and realizing there were no new treatments. The person in front of me was not likely to be here two months, three months, four months down the line.
We had very bad luck for the first 16 years of the AIDS epidemic until we saw how the advent of highly active antiretroviral therapy, and it was one disappointment after another, as much as we kept fighting.
Kai: That uncertainty about where science would go and how fast, on a different scale, at least it feels certainly how a lot of people felt this summer as the hospitals on the East Coast filled up, at least from COVID. Did it seem familiar to you at the time? Or are these apples and oranges?
Gregg: No. It still feels familiar. The weird thing for me is that the care of not knowing if you catch it, you'll survive, thinking about when there's going to be an effective treatment, when there's going to be a vaccine, all of a sudden we into flashback mode. This wasn't just happening to the LGBTQ community, communities of color, people use drugs, et cetera, it was happening to an entire world. It was just a different kind of scale of experience, which I thought after going through the AIDS epidemic, nothing could compete with that but the past 10, 11 months have been just quite a ride.
Kai: Quite a ride. It's certainly a flashback for me and I wasn't an adult in the '80s and so I wasn't losing friends in the immediate way, but the people that I knew and then lost in the '90s, I found it very difficult to separate emotionally the two events.
Gregg: No, I agree. It's hard.
Kai: What's certainly not similar though to the HIV/AIDS pandemic is how rapidly science has in fact moved on COVID. It's worth pointing out that there is still no vaccine for HIV and honestly I've said a couple of times in this hour as a Black man, as a gay man, I feel some way about that fact. I wonder talking to you, is that even fair of me? Am I comparing things incorrectly?
Gregg: It's remarkable to me that at the end of the year, we're going to have multiple COVID-19 vaccines approved by the FDA and we're still waiting for an AIDS vaccine. I feel enormous anger still, that we didn't have an Operation Warp Speed for us back in the '80s and '90s and that, as much as Trump botched the response to the COVID-19 epidemic, there has been a wholesale mobilization across the United States to find a vaccine, at least. I feel like, "What about us? What happened back in the '80s and '90s that said we weren't worth the fight?"
Kai: I'm talking with Gregg Gonsalves about how his 30 years of AIDS activism, colors his view of the COVID-19 pandemic. Gregg, you're joining us from New Haven, Connecticut, that area of the state stretching up from New York City through the suburbs. It's often called one of the most unequal places in the country in terms of income and wealth, at least, and that certainly tracks with race as well. You've talked about this kind of inequality and how it shaped healthcare over the generations. How do you think it shaped the political response to HIV that we're now talking about?
Gregg: I think you have to go way back past COVID, past HIV, You have to dig deeper into American history to figure out how we got to where we are today. There was an article by Jeneen Interlandi, who is on the editorial board of the New York Times in those 16, 19 issues of the New York Times magazine last year called Why Doesn't America Have National Health Care? It has everything to do with race.
She talks in that article about how after the Civil War, smallpox was raging through the American South and former slave owners were wondering, "Should we do something? We want to save these people mostly because we can lure them back on the plantations to work for us. We don't want them to be too healthy because otherwise, they may have set the political balance to the American South."
A guy named Jim Downs, who was a professor at the University of Connecticut, which is now at Gettysburg College, wrote in this book called Dying for Freedom that healthcare in America represented white ambivalence at every turn. If you start thinking about that through the new deal programs where African-Americans were excluded from those benefits to the Hill-Burton Act, when they expanded hospitals in the South, in the '40s and '50s under this express agreement that Southern governors could pick where those hospitals went and guess where they went, all the way through the '80s and '90s, you realize we've been playing in the white ambivalence at every turn.
Every time there's a health crisis in America, race comes up and we ask, "Who's getting infected? Who's affected? Who matters?" We saw that in AIDS and we've seen it in COVID-19. It's a legacy that stretches way, way back, past the 20th century into the 19th and probably before that for us.
Kai: I wonder about how that same thing then when we think about COVID. I have to say there was a time, at least this summer, when it felt like the Trump administration's denial of what was going on was tied up in his dismissal and fear-mongering of cities, which is to say Black people, immigrants, gays, and the like. Does that feel accurate too?
Gregg: Oh yes. I don't know if he said it or I just imagine him saying it, but is it our people who are getting infected? I don't think he felt like it was the people who mattered to him, who were getting infected during the past 8 to 10, 11 months that we've been living with this disease but I think his pathology is so much more deep and inhumane in that, he can care less who else gets it. He's always racist, misogynist, and a homophobe, but his narcissism is so deep that the world could burn down around him and he wouldn't really give a damn.
Kai: Let's go to Louie in Bed-Stuy. Louie, welcome to the show.
Louie: Hi Kai. I was diagnosed in '86, December 1986. Suffered with AIDS for years, and a member of ACT UP New York. Now I’m HIV undetectable and, Hep C cured, a former heroin user. In July of this year, I caught COVID and wow, I can't believe I survived it.
Kai: Were you hospitalized?
Louie: Yes I was in Brooklyn Hospital. I had the best doctors, the same doctors who've been giving me care with my treatment, even living with HIV and also the cure for Hep-C as well. I was co-infected. I was a member of ACT UP. There was a ACT UP member I'd go to over and over again. His name was Vito Russo. He said, "Someday, the AIDS crisis-" and I put it in the COVID crisis, "-will end. And when that time has come and gone, there will be people on the planet, Black people, white people, gay and straight, who will have remembered that there was once a terrible disease and that there were a group of people who were moved to stand up, act up and fight back. And some of them died so the others may live and be free."
Kai: Thank you for that remembrance, Louie. And I'm so happy that you were able to overcome both diagnoses. Can I ask you quickly before I let you go? When thinking about being diagnosed with HIV in 1986, when there wasn't treatment available and then COVID this summer when also a lot of people were dying from it, I just wonder how you felt emotionally with those two things. How did you deal with that uncertainty?
Louie: I was fortunate to have a network. I belong to a network VOCAL New York, Voices Of Community Advocates and Leaders and so being connected was so important to my resilience. Emotionally, yes, I had my moments. It's okay to cry even though your friend is dying.
Kai: Yes, it is.
Louie: I was very just fortunate that I'd twice a week go out to- with a team. We'd go to high-drug trafficking areas in Bed-Stuy and Williamsburg and Red Hook and reach out, do outreach providing masks for people that homeless on the streets or just being released from prison and getting them connected into detoxes, and spreading the word that there's hope.
Kai: Louie, thank you for that work and for your testimony. Thanks for calling. Gregg, one of the things that we've heard is that COVID is so much more difficult for people with compromised immune systems. Has there been any research or any thought about what it means for people who are HIV positive?
Gregg: I think the main point is that if you're suppressed in antiretroviral therapy, you should be treated as any other patient coming into a hospital. You shouldn't be considered at higher risk than probably people of your own age group. People living with HIV have an uncontrolled virus and have frank immunosuppression. I think that's another story, but if you're controlled on antiretroviral therapy, nobody's suggesting that you should have a different outcome with COVID than your HIV negative peers.
Kai: Which is just a testament to how far science has come, at least on the treatment side if not the distribution of those treatments.
Gregg: Exactly.
Kai: Back on a personal note for you. I understand that 1995 was really a tough year for you. Can you take us back there? I feel like there's a lot of people facing similarly intense grief right now and I just wanted to hear how you faced that onslaught.
Gregg: That year, I lost my cousin who basically grew up around the corner in my neighborhood growing up on Long Island and lost a good friend of mine, Jay Funk, who was the former boyfriend of my former boyfriend but tended to two people dying in 1995 and in the midst of it, finding out my own diagnosis. This is months just before we get the news of highly active antiretroviral therapy emerging on the scene.
As you, the previous segment from earlier in the show, said, just a few more months and something will happen and few more months, it'll happen. They could have beaten it too. So to find my own diagnosis happening on the cusp of the antiretroviral treatment for HIV, it was a miracle for me, but there's no shortage of guilt that the people I loved, if they just had been able to hang on for a few more months, they might be with us here today.
Kai: Guilt, you say?
Gregg: I don't know. Why did I survive? Why did all my friends survive? Not all of them, but there's a bunch of my friends, Peter Staley, David Barr, others who survived this against all odds. And yes, we had great healthcare but the just inordinate amount of loss we all faced, you start to think like, "Why me? Why did I survive this when so many beautiful, wonderful people who enriched our world - like the profile of the young man you featured earlier in the show - are gone from us forever?"
Kai: Hey everybody. I want to ask your help with something. A huge part of what we're doing with this show is building a community, a community of people who want to share the joy and the work of creating and living in a healthy plural society. That's why we've started taking calls on the live show and soliciting your tweets and your voicemails here.
Michael: Hey, this is Michael from Raleigh, North Carolina.
Ida: This is Ida in Austin, Texas.
Dorian: Hi Kai, my name is Dorian from Queens, New York.
Caller 4: My wildest dreams and imaginations. It's going to be hard for me to get through this note to you guys without getting emotional.
Kai: It's all part of building a community and you can do two things to help build our community. First off, just invite somebody to join you in it. Maybe even start listening together on Sunday evenings, but however you do it, invite other people in.
Second, you can leave a review on whatever app you're using to listen right now. You can give us a rating there. That's nice but also leave a comment. Why do you listen? Why should others join you in listening? Again, think of it as making an invitation. It's how a community works. So thanks in advance for doing either or both of those things, and even if you can't do either of them, thanks for being part of our community.
[music]
Welcome back. This is the United States of Anxiety, and I'm Kai Wright. This week, we are asking what we can learn from the nearly 40-year-old HIV/AIDS pandemic, as we approach one year of living with COVID-19. I'm joined by Gregg Gonsalves, who is co-director of the Global Health Justice Partnership at Yale University and has been an AIDS activist for three decades. Gregg, let's get one more caller in here, Paul who's in the financial district. Paul, welcome to the show.
Paul: Hi, how are you, Kai?
Kai: I'm good. Do you have a memory of that time of the early HIV epidemic that you want to share?
Paul: I work in the film industry now. I was working in the restaurant industry in Chelsea and living in Chelsea at the time, and my mom worked at St Vincent's Hospital. The parallel of course is now that my daughter is a nurse in Langone. The similarity of stories that I'm hearing and the terror and the fear that they were both experiencing working in the health industry at the time is kind of shocking.
The stories my mom would tell me about how people were afraid of bringing, putting food into the rooms at St. Vincent's of the AIDS patients, and that same similar terror that my daughter's experiencing really sort of, I feel like it's a strange experience of going full circle, but in a horrible way.
Kai: Thank you for that, Paul. Gregg, I want to ask you because one of the things that-- there's a lot of these very difficult memories of the HIV epidemic that are resonant right now, but part of why I wanted to talk to you is I find there are a number of things that are quite inspiring about that period to me. I want to ask you about that because you were present at a time when a group of people in our community said, "You know what? We'll take care of ourselves. We will force the power that exists to value our lives." I just wonder about that now. Where do we see that connection with COVID now?
Gregg: Actually in New York City you do see it because there's something called the COVID-19 Working Group, maybe not as visible as ACT UP New York, but it has a lot of the alumnus from ACT UP New York and some younger folks, also some of the researchers from the time of the '80s and '90s during on HIV that are all working together to think about how to improve both local policy in the city, but also national policy, re-switch treatment testing, all the things, to focus back in the '80s and '90s around HIV.
It's an infectious disease. All the infectious disease docs from the '80s who are still around doing this work are on the frontline for COVID, but also the people who remember the AIDS epidemic, activist groups like Rise and Resist in New York, and others have mobilized themselves around COVID-19. It's not a surprise that it's the old ACT UP and the new generation aligned with them that are stepping up both in New York City, but also around the country.
Kai: On that score, thinking about all the treatment activism, both the past and present in HIV, and then thinking about the period we're now entering with vaccine rollout, what are lessons there? Because we've now got these very promising vaccines. You've written, you wrote in The Nation that you don't expect them to be a big part of our rollout, of our dealing with COVID-19 at least for much of 2021. Do you still think that's true? If so, why? How does it relate to what we've seen in the past in dealing with pharmaceutical companies?
Gregg: I would revise my opinion and say, they're going to be an important feature of the next year, but the devil is not in the vaccines themselves but in the distribution. The point is that vaccines are only as good as a shot in the arm to the people who need to get it. One of the lessons of the advent of highly active antiretroviral therapy is that when certain people get access to things, they figure out other people.
Andrew Sullivan wrote an article in New York Times magazine in the mid-1990s saying when plagues end which meant AIDS was over for him and for a generation of gay white men, they took their antiretroviral pills, they took their health insurance and went home. Are we going to see a similar two-tiered retreat for COVID-19 in which certain segments of our population get access to the vaccine while we let pockets of the virus persist into 2022, 2023, because the vaccine will just reach there in time which is never a penetration.
Kai: What do you see now, or look for in the Biden administration to make sure that's not happening? That Andrew Sullivan, 1996 article really defined the next 10 years of my life in trying to respond to it in the Black community. What do you see? What are you looking for to make sure we are not back in that place?
Gregg: One is that we're talking about, should nursing home residents, should health care workers get access to the vaccine? The point is that across the age demographics and the settings like nursing homes we have to admit, it's just a matter of pure fact that the virus covered different kinds of swaths of communities of color in the United States.
We're going to have to figure out a way to make sure that equity is part of what the Biden administration does when it rolls out vaccines.
I'm happy that my colleague here at Yale, Marcella Nunez-Smith, who has worked on health equity all her life is going to take up a post with the new Biden administration specifically on health equity. I'm hoping that that's a sign that the administration is going to be putting equity in access to vaccines and any of these interventions we put in place for COVID-19 front and center which we didn't necessarily see in the 1990s, in the United States for antiretroviral treatment.
Kai: What about the potential reluctance of people to take the vaccines? We see survey data that suggests African-Americans in particular might be reluctant. We spent a lot of years fighting this information in the Black community about HIV. Where do you see that headed?
Gregg: It's going to be an issue. It's not just people in the African-American community. There was a big poll of New York City police officers, and half of them said they wouldn't take it. And so we have a big uphill job to do to get people to take the vaccine and as we learned from HIV, peer-based education is the best way to go. Yes, the White House can use bully pulpit of the presidency to make the case that everybody should take a jab in the arm, but we're going to have to build a legion of community health workers that are in the communities that are part of the communities they come from to help vaccinate people, to help educate people, to help them through the next few months. The point is, is that it's going to have to be from the bottom-up, but not necessarily just from the top-down. We can have all the best-laid plans to get vaccines out the door, but the rubber hits the road in neighborhoods in New York City, in New Haven, where people have struggled to get access to healthcare on an equal basis for many, many years. So the vaccine coming along doesn't necessarily mean it's going to get to them with great speed or efficiency.
Kai: Last 30 seconds. Any parting thoughts for people about what we're going to face now for the next coming months with COVID?
Gregg: It's going to be really rough. The vaccine and the immunity that we might all get by it is something for thinking of the summer of 2021. Keep your masks on. Keep your distance. The holidays are coming. If you can pass up this Christmas, Hanukkah, and Kwanzaa, do it because we all want to be around for next year, so we can be together again.
Kai: Gregg Gonsalves is co-director of the Global Health Justice Partnership at Yale University. He's been an AIDS activist for three decades. You can follow his writing on COVID-19 at The Nation Magazine. Gregg, thanks for joining us.
Gregg: Anytime, Kai.
[music]
Kai: United States of Anxiety is a production of WNYC Studios. A special thanks to the family of Michael Calvert for opening themselves and their hearts to us when we reached out all these years after his death, I know that had to be tough. Thanks for allowing us to share him with our community here on the show. Jared Paul mixed the podcast version this week, Kevin Bristow and Matthew Marando were at the boards for the live show. Special thanks to Ed Haber for his technical assistance making Karen's 1986 recording work for a digital world.
Our team also includes Carolyn Adams, Emily Botein, Jenny Casas, Marianne McCune, Christopher Werth, and Veralyn Williams. Our theme music was written by Hannis Brown and performed by the Outer Borough Brass Band. Karen Frillmann is our Executive Producer, and I am Kai Wright.
You can keep in touch with me on Twitter @kai_wright. As always, I hope you'll join us for the live version of the show next Sunday, 6:00 PM, Eastern. You can stream it at wnyc.org or tell your smart speaker to play WNYC. Until then, thanks for listening. Take care of yourselves.
[END OF AUDIO]
Copyright © 2020 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.